Introduction
Physical therapy in Asheville for Upper Back and Neck
Welcome to Combined Therapy Specialties patient resource about Cervical Discectomy.
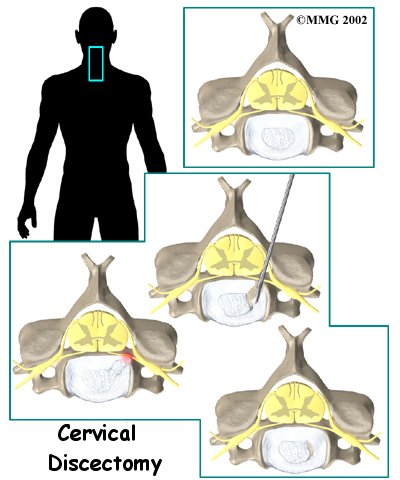
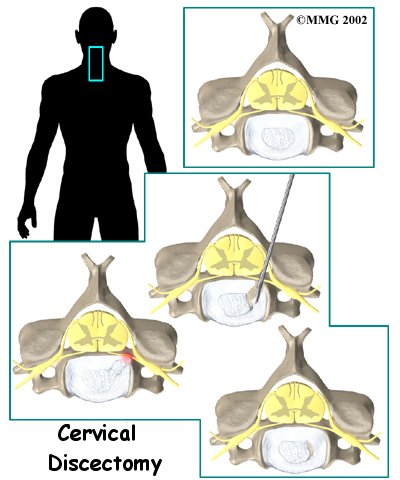
Cervical discectomy is surgery to remove one or more discs from the neck. The disc is the pad that separates the neck vertebrae; ectomy means to take out. Usually a discectomy is combined with a fusion of the two vertebrae that are separated by the disc. In some cases, this procedure is done without a fusion. A cervical discectomy without a fusion may be suggested for younger patients between 20 and 45 years old who have symptoms due to a herniated disc.
This article will help you understand:
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect during your recovery
Anatomy
What parts of the neck are involved?
Surgeons usually perform this procedure through the front of the neck. This is called the neck region. Key structures include ligaments, bones, intervertebral discs, spinal cord, spinal nerves and the neural foramina.
Surgery is occasionally done through the back, or posterior region, of the neck. Important structures in this area include the ligaments and bones, especially the lamina bones.
Related Document: Combined Therapy Specialties Guide to Cervical Spine Anatomy
Rationale
What do surgeons hope to achieve?
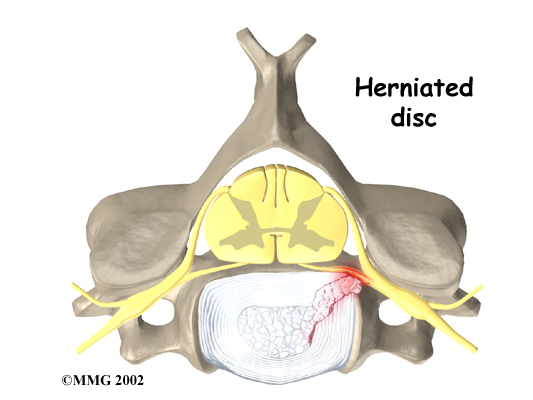
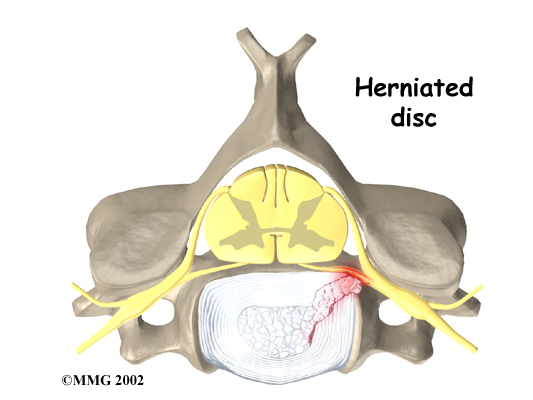 Discectomy is used to alleviate symptoms of a . A disc herniation happens when the nucleus inside the center of the disc pushes through the annulus, the ligaments surrounding the nucleus. The herniated disc material may push outward, causing pain. Numbness or weakness in the arm occurs when the nucleus pushes on the spinal nerve root. Of greater concern is a condition in which the nucleus herniates straight backward into the spinal cord, called a central herniation. Discectomy relieves pressure on the ligaments, nerves, or spinal cord.
Discectomy is used to alleviate symptoms of a . A disc herniation happens when the nucleus inside the center of the disc pushes through the annulus, the ligaments surrounding the nucleus. The herniated disc material may push outward, causing pain. Numbness or weakness in the arm occurs when the nucleus pushes on the spinal nerve root. Of greater concern is a condition in which the nucleus herniates straight backward into the spinal cord, called a central herniation. Discectomy relieves pressure on the ligaments, nerves, or spinal cord.
Discectomy is also commonly used when the surgeon plans to fuse the bones of two neck vertebrae into one solid bone. Most surgeons will take the disc out and replace the empty space with a block of bone graft, a procedure called cervical fusion.
Discectomy alone is usually only used for younger patients (20 to 45 years old) whose symptoms are from herniation of the disc. But some surgeons think discectomy should always be combined with fusion of the bones above and below. They are concerned that the empty space where the disc was removed may eventually collapse and fill in with bone. Inserting a bone block during fusion surgery helps keep pressure off the spinal nerves because the graft widens the neural foramina. The neural foramina are openings on each side of the vertebrae where nerves exit the spinal canal. Most research on discectomy by itself shows good short-term benefits compared to discectomy with fusion. But more information is needed about whether the long-term results are equally as good.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Cervical discectomy is commonly done through the (front) of the neck. This is called anterior cervical discectomy. However, when many pieces of the herniated disc have squeezed into the posterior (back) of the spine, surgeons may need to operate through the back of the neck using a procedure called posterior cervical discectomy.
Patients are given a general anesthesia to put them to sleep during most spine surgeries. As you sleep, your breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
Anterior Discectomy
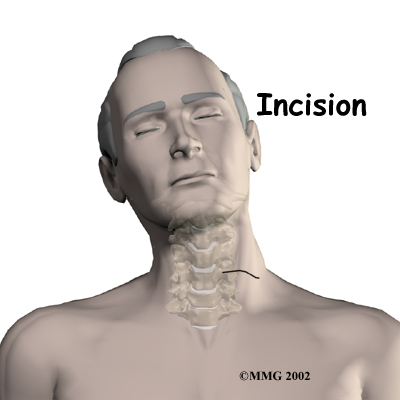
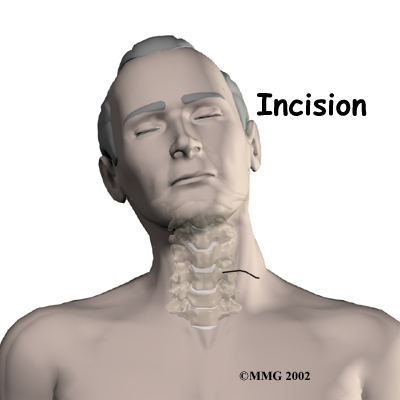
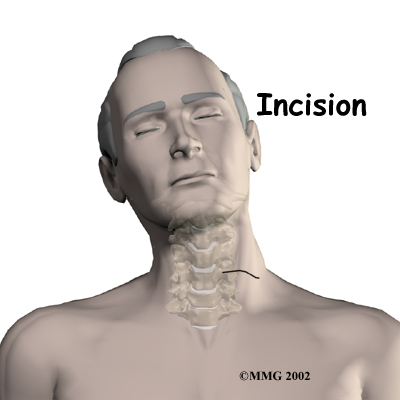
The patient's neck is positioned facing the ceiling with the head bent back and turned slightly to the right. A two-inch incision is made two to three fingers' width above the collar bone across the left-hand side of the neck. The left side is chosen to avoid injuring the nerve going to the voice box. Retractors are used to gently separate and hold the neck muscles and soft tissues apart so the surgeon can work on the front of the spine.
A needle is inserted into the herniated disc, and an X-ray is taken to identify and confirm it is the correct disc. A long strip of muscle and the anterior longitudinal ligament that cover the front of the vertebral bodies are carefully pulled to the side. Forceps are used to take out the front half of the disc. Next a small rotary cutting tool (a burr) is used to carefully remove the back half of the disc. A surgical microscope is used to help the surgeon see and remove pieces of disc material and any bone spurs that are near the spinal cord.
The muscles and soft tissues are put back in place, and the skin is stitched together.
 Posterior Discectomy
Posterior Discectomy
This method is used when the herniated disc has fragmented into small pieces near the spinal nerve.
The operation is usually done with the patient lying face down with the neck bent forward and held in a headrest. The surgeon makes a short incision down the center of the back of the neck. The skin and soft tissues are separated to expose the bones along the back of the spine.
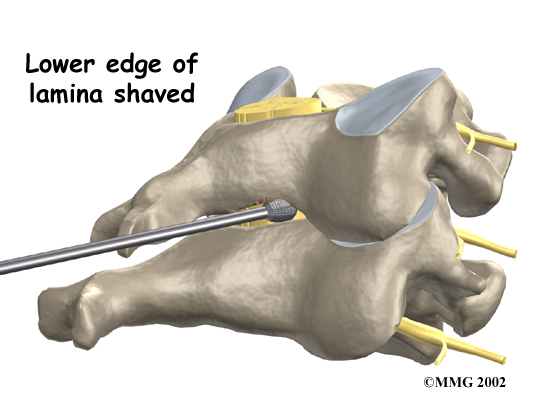
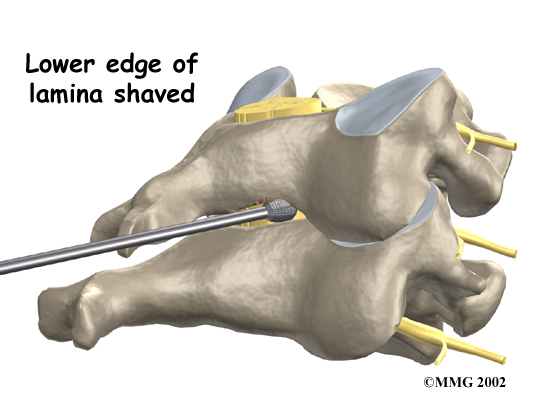
Then the surgeon may use an X-ray to identify the injured disc. A burr is used to , the back part of the ring over the spinal cord. When the disc has jutted straight backward into the spinal cord (central herniation), surgeons may need to completely remove both lamina bones in order to see better and to be able to clear all the pieces of the disc near the spinal cord.
Related Document: client_company*s Guide to Cervical Laminectomy
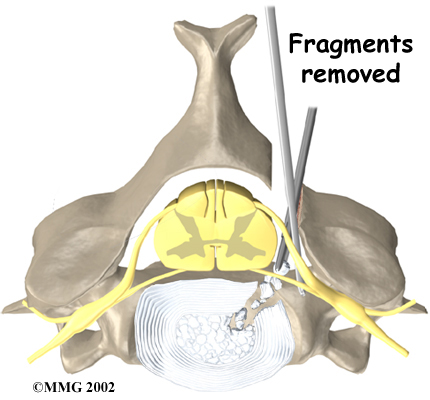
After shaving the lamina bone, the surgeon cuts a small opening in the ligamentum flavum, a ligament within the spinal canal and in front of the lamina bone. By removing part of this ligament, the surgeon exposes the spot where the disc fragments are pressed against the spinal nerve. Next, the spinal nerve is gently moved upward. Using a surgical microscope, the surgeon magnifies the area in order to carefully and any bone spurs.
The muscles and soft tissues are put back in place, and the skin is stitched together.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following discectomy include:
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- ongoing pain
This is not intended to be a complete list of the possible complications, but these are the most common.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include:
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Nerve Damage
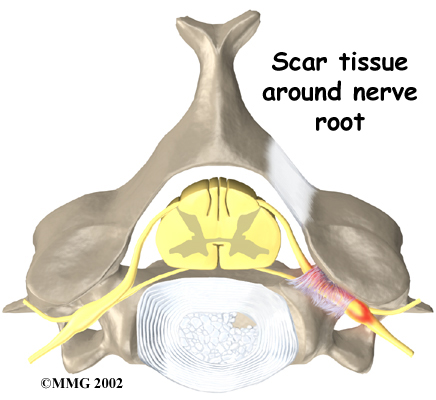 Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of . An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of . An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. When doing anterior neck surgery, surgeons prefer to go through the left side of the neck where the path of the nerve to the voice box is more predictable than on the right side. During surgery, the nerve may get stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases where the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Ongoing Pain
Many patients get nearly complete relief of symptoms from the discectomy procedure. As with any surgery, however, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients are usually able to get out of bed within an hour or two after surgery. Your surgeon may have you wear a hard or soft neck collar. If not, you will be instructed to move your neck only carefully and comfortably.
Most patients leave the hospital the day after surgery and are safe to drive within a week or two. People generally get back to light work by four weeks and can do heavier work and sports within two to three months.
Outpatient physical therapy is usually prescribed only for patients who have extra pain or show significant muscle weakness and deconditioning.
Our Rehabilitation
What should I expect as I recover?
After routine cervical discectomy surgery, you may participate in a short period of physical therapy at Combined Therapy Specialties if you have lost muscle tone in the shoulder or arm, have problems controlling pain, or need guidance about returning to heavier types of work.
Although the time required for recovery varies, you will probably only need to attend physical therapy sessions for two to four weeks, and should expect full recovery to take up to three months.
At first, our physical therapy treatments are used to help control pain and inflammation. Our physical therapist may use ice, electrical stimulation, massage and other hands-on treatments to ease muscle spasm and pain.
We then slowly add active treatments. These include exercises for improving heart and lung function. Walking, stationary cycling, and arm cycling are ideal cardiovascular exercises. Our physical therapists also teach specific exercises to help tone and control the muscles that stabilize your neck and upper back.
We will also work with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. This training helps you keep your neck in safe positions as you go about your work and daily activities. We'll teach you how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
As your condition improves, our physical therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. Our therapist may suggest changes in job tasks that enable you to go back to your previous job. We can also provide ideas for alternate forms of work. You'll learn to do your tasks in ways that keep your neck safe and free of extra strain.
Before your physical therapy sessions end, our physical therapist will teach you a number of ways to avoid future problems.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Portions of this document copyright MMG, LLC.







 Discectomy is used to alleviate symptoms of a
Discectomy is used to alleviate symptoms of a 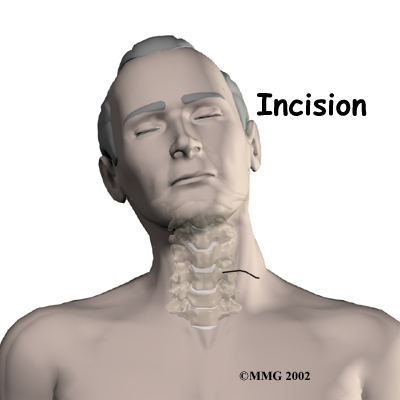
 Posterior Discectomy
Posterior Discectomy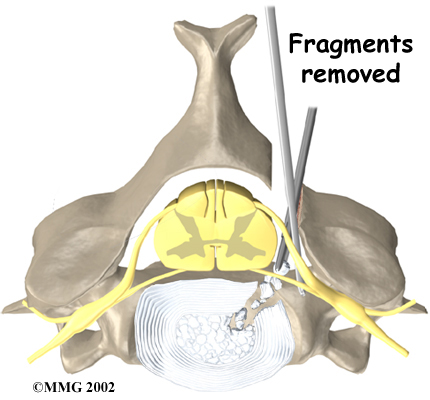
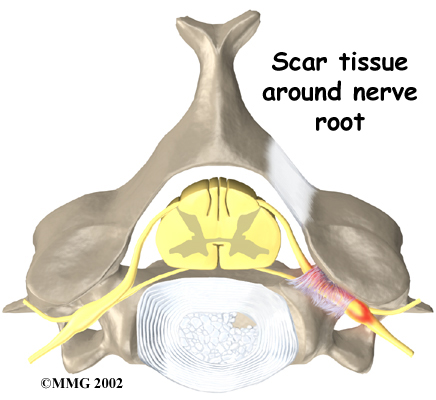 Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of 
