Introduction
Physical therapy in Asheville for Upper Back and Neck
Welcome to Combined Therapy Specialties patient resource about Cervical Artificial Disc Replacement.
Artificial disc replacement (ADR) is relatively new. In June 2004, the first ADR for the lumbar spine (low back) was approved by the FDA for use in the US. Replacing a damaged disc in the cervical spine (neck) is a bit trickier. The disc is part of a complex joint in the spine. Making a replacement disc that works and that will last is not an easy task. Cervical artificial disc replacement devices are currently undergoing study for FDA approval in the United States.
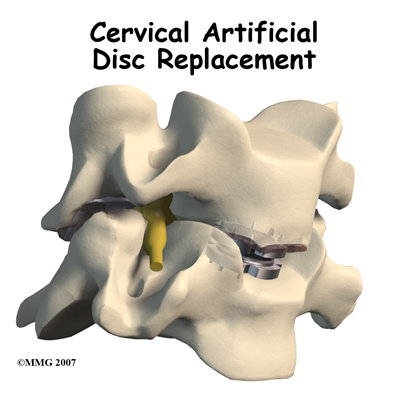
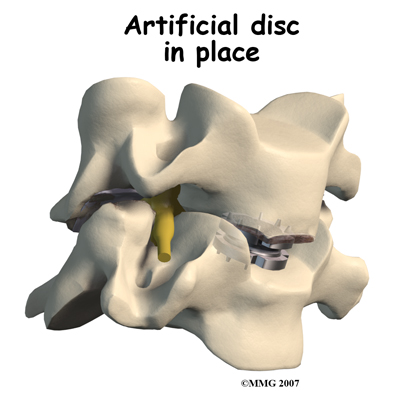
The artificial disc is inserted in the space between two vertebrae. The goal is to replace the diseased or damaged disc while keeping your normal neck motion. The hope is that your spine will be protected from similar problems above and below the affected spinal level.
This guide will help you understand:
- what parts of the spine are involved
- what your surgeon hopes to achieve
- who can benefit from this procedure
- how do I prepare for surgery
- what happens during the procedure
- what to expect as you recover
Anatomy
What parts of the spine are invovled?
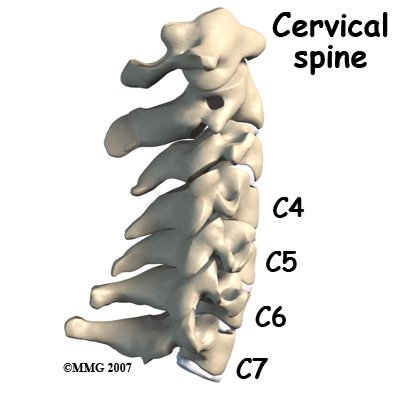
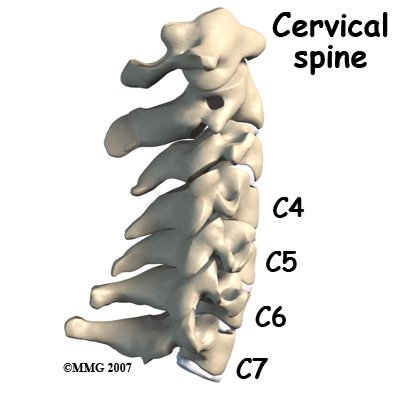
Disc replacement typically occurs at cervical spine levels C4-5, C5-6, or C6-7. The first seven vertebrae make up the cervical spine. Doctors often refer to these vertebrae as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine (the chest area) at the first thoracic vertebra, T1.
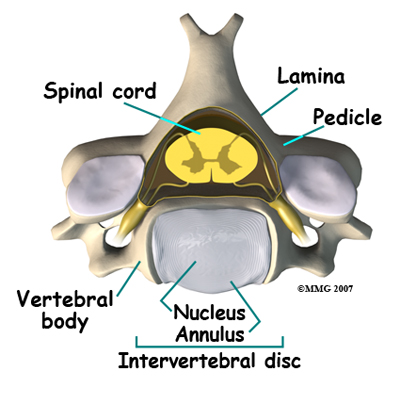
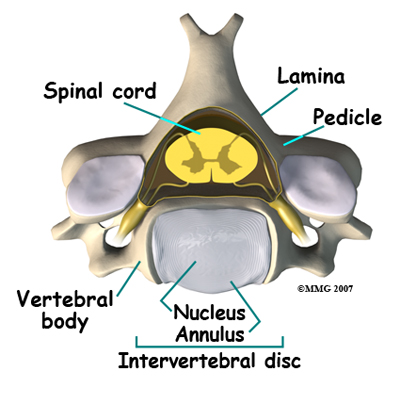
Each vertebra is made of the same parts. The main section of each cervical vertebrae, from C2 to C7, is formed by a round block of bone, called the. A bony ring attaches to the back of the vertebral body. This ring has two parts. Two pedicles connect directly to the back of the vertebral body. Two lamina bones join the pedicles to complete the ring. The lamina bones form the outer rim of the bony ring. When the vertebrae are stacked on top of each other, the bony rings form a hollow tube that surrounds the spinal cord. The laminae provide a protective wall around the spinal cord.
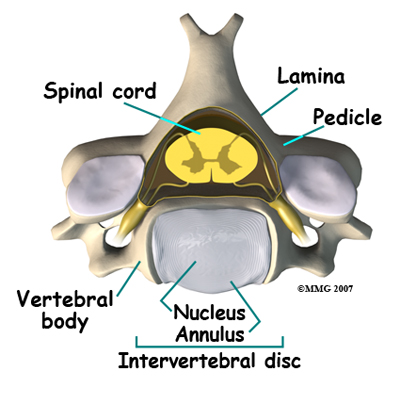
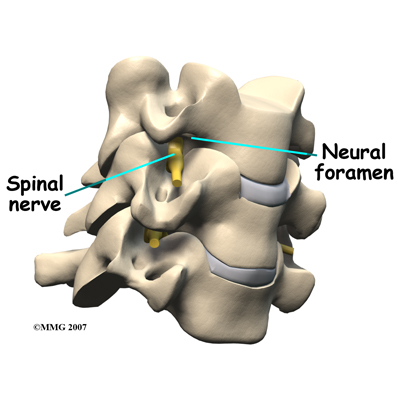
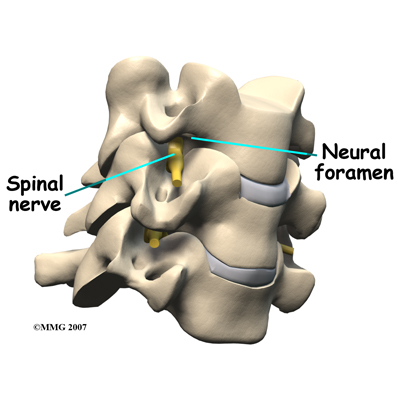
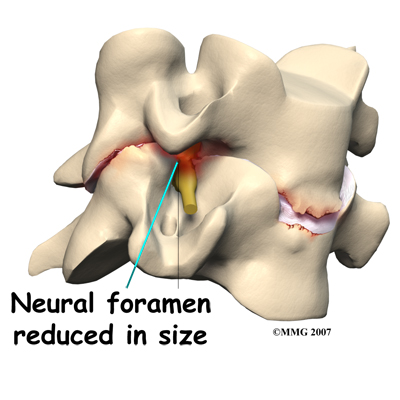
On the left and right side of each vertebra is a small tunnel called a neural foramen. (Foramina is the plural term.) The two nerves that leave the spine at each vertebra go through the foramina, one on the left and one on the right. The intervertebral disc sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits behind the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
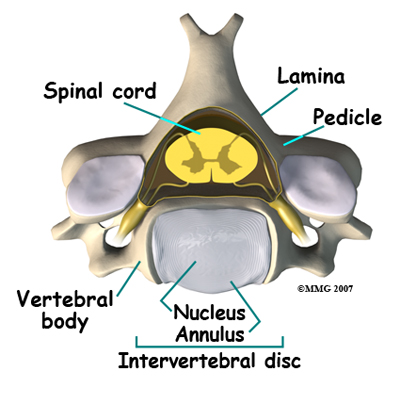
A special type of structure in the spine called an intervertebral disc has two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption in the spine. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it.
Related Document: Combined Therapy Specialties Guide to Cervical Spine Anatomy
Rationale
What does the surgeon hope to achieve?
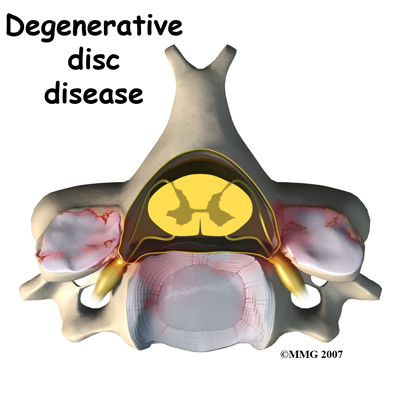
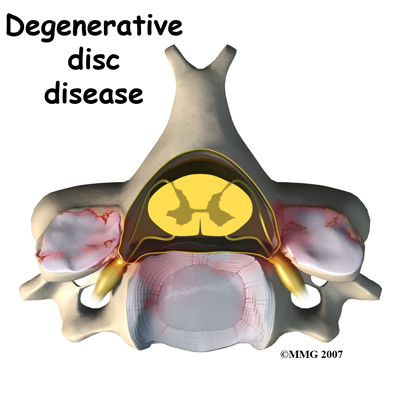
Disc replacement surgery is done to stop the symptoms of degenerative disc disease. Discs wear out or degenerate as a natural part of aging and from stress and strain on the neck. Eventually, the problem disc collapses. This causes the vertebra above to sink toward the one below. This loss of disc height affects the nearby structures – especially the facet joints.
When the disc collapses, it no longer supports its share of the load in the cervical spine. The facet joints of the spine begin to support more of the force that is transmitted between each vertebra. This increases the wear and tear on the articular cartilage that covers the surface of the joints. The articular cartilage is the smooth, slippery surface that covers the surface of the bone in any joint in the body. Articular cartilage is tough, but it does not tolerate abnormal pressure well for long. When damaged, articular cartilage does not have the ability to heal. This wear and tear is what is commonly referred to as arthritis.
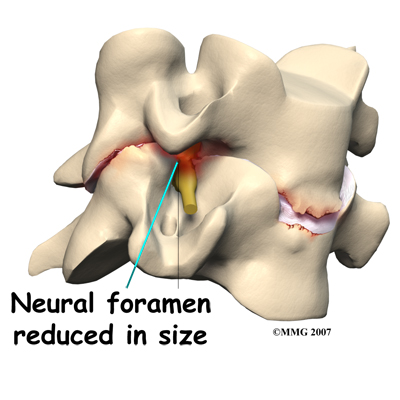
Shrinking disc height also reduces the size of the neural foramina, the openings between each vertebral pair where the nerve roots leave the spinal column. The arthritis also results in the development of bone spurs that may protrude into these openings, further narrowing the space that the nerves have to exit the spinal canal. The nerve roots can end up getting squeezed where they pass through the neural foramina.
The traditional way of treating severe neck pain caused by disc degeneration is a procedure called an anterior cervical discectomy and fusion. In this procedure, the surgeon makes an incision in the anterior (front) of the neck, performs a discectomy (removes the disc) and fuses the two vertebrae together. A fusion simply means that two bones grow together. Usually, when two vertebrae are fused together, a small piece of bone called a bone graft is inserted between the two vertebrae where the disc has been removed. This bone graft serves to both separate the vertebrae and to stimulate the two bones to grow together - or fuse.
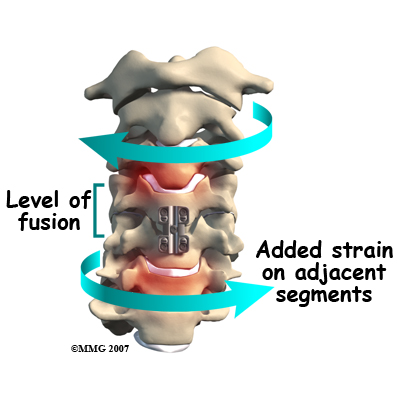
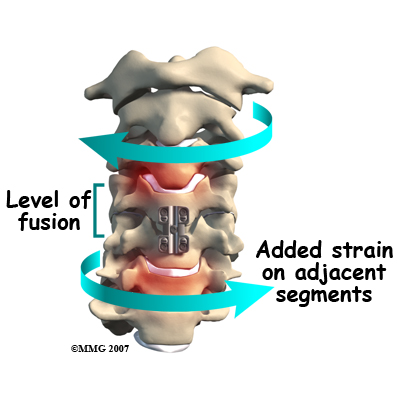
The fusion procedure usually involves the use of hardware, such as screws, plates, or cages to keep the bones from moving. Fusion restricts movement in the problem area, but it creates greater strain on the healthy spinal segments above and below. The added strain may eventually cause these segments to wear out. This is called adjacent-segment degeneration.
Replacing the damaged disc with an artificial disc, or implant, called a prosthesis can restore the normal distance between the two vertebrae. The artificial disc sits between the two vertebrae and "jacks up" the upper vertebra. Enlarging the disc space relieves pressure on the facet joints. It also opens up the space around the spinal nerve roots where they pass through the neural foramina.
Another benefit of the artificial disc replacement is that it mimics a healthy disc. Natural motion is preserved in the spine where the new disc is implanted. And it helps maintain stability in the spinal joints above and below it.
Who can benefit from this procedure
The indications for a cervical disc replacement are generally the same as for a cervical discectomy and fusion. A person must have symptoms from a cervical disc problem. Symptoms include neck and/or arm pain, arm weakness, or arm and hand numbness. These symptoms may be due to a herniated disc and/or bone spurs called osteophytes pressing on adjacent nerves or the spinal cord. This condition typically occurs at cervical spine levels C4-5, C5-6, or C6-7.
Artificial disc replacement is still somewhat experimental in the United States. Patients are only having this type of surgery as part of a clinical trial. A clinical trial is a type of research where a drug or device is being tested in real patients in a very controlled way. In the United States, surgeons are currently only replacing one cervical disc in a patient's cervical spine at this time. In Europe, surgeons are replacing more than one disc. Surgeons in the United States may be cleared for replacing more than one cervical disc in the near future.
Prior to being admitted into a clinical trial, the patient must meet strict defined entrance criteria. The patient must have completed a trial of conservative (non-operative) treatment for at least four to six weeks, usually consisting of anti-inflammatory medication and intense physical therapy. The patient must have no history of previous neck surgery and the patient must be determined by the surgeon conducting the research to be a good surgical candidate for the ADR.
Cervical artificial disc replacement is indicated for the treatment of radiculopathy (pressure on the spinal nerve) and myelopathy (pressure on the spinal cord) at one or two levels. In the future, it may be used for the treatment of three or more symptomatic levels or levels adjacent to a cervical spine fusion. This use is still under investigation.
More data is needed before the uses of cervical artificial disc replacements are expanded to other problems in the cervical spine. Cervical artificial disc replacement is not advised when there is cervical spine instability, significant facet joint damage, or infection.
Preparation
How should I prepare for surgery?
Your spine surgeon will gather a variety of information before recommending disc replacement surgery. In addition to taking a history and doing a physical exam, your surgeon may order various diagnostic studies, such as x-rays, magnetic resonance imaging (MRI) scans, CT scans, or discograms.
Once you and your surgeon have agreed that disc replacement surgery is indicated, certain preparations for the surgery are important. Your doctor may tell you to be NPO for a certain amount of time before the procedure. This means that you should not eat or drink anything for a certain amount of time before your procedure. This means no water, no coffee, no tea - not anything. You may receive special instructions to take your usual medications with a small amount of water. Check with your doctor if you are unsure what to do.
You should tell your doctor if you are taking any medications that thin your blood or interfere with blood clotting. The most common blood thinner is Coumadin. Other medications also slow down blood clotting. Aspirin, ibuprofen, and nearly all of the anti-inflammatory medications affect blood clotting. So do medications used to prevent strokes such as Plavix. These medications usually need to be stopped seven days prior to the procedure. Be sure to let your doctor know if you are on any of these medications.
You should stop smoking or using tobacco in any form as soon as possible before surgery. This is very important to reduce complications from heart and lung problems. Tobacco use, especially smoking, also decreases the success rate of spine surgery. Stopping smoking will increase your chances of a successful result.
Discussions will be held with your family and people who may be assisting you once you return from the hospital. You may need to visit your primary care physician or internal medicine specialist to obtain medical clearance for surgery. This will ensure that you are in the best medical condition possible prior to the surgery.
Hospitals often have preoperative teaching for patients undergoing major spinal operations. These teaching sessions can help you understand what to expect both while you are in the hospital and after you return home. A doctor who will be performing your anesthesia (an anesthesiologist) will evaluate and counsel you regarding anesthesia.
Surgical Procedure
What happens during the operation?
Before we describe the procedure, let's look first at the artificial disc itself.
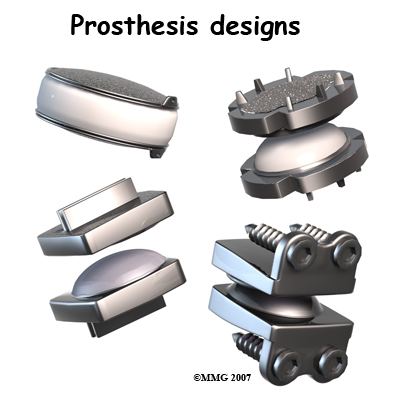
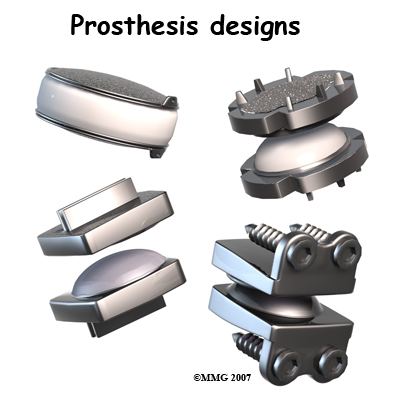
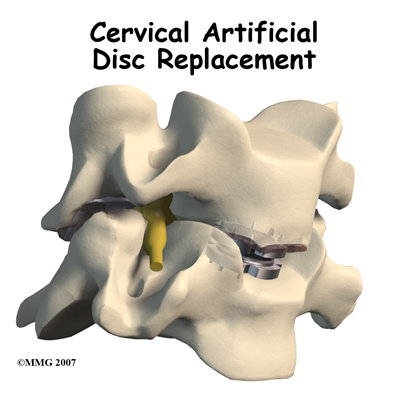
The cervical artificial disc has several different designs. Some look like a sandwich with two endplates separated by a plastic spacer. The two endplates are made of cobalt chromium alloy, a safe material that has been used for many years in replacement joints for the hip and knee.
A plastic (polyethylene) core fits in between the two metal endplates. The core acts as a spacer and is shaped so that the endplates pivot in a way that imitates normal motion of the two vertebrae. There are small prongs on one side of each endplate. The prongs help anchor the endplate to the surface of the vertebral body.
Another artificial disc replacement design is a ball and socket articulation to allow for normal translation of motion at that segment. The implant may be made of titanium and polyurethane in a metal-on-plastic design. Some are made of stainless steel and are all metal-on-metal.
Inserted between two vertebrae, the prosthesis reestablishes the height between two vertebrae. As a result of enlarging the disc space, the nearby spinal ligaments are pulled tight, which helps hold the prosthesis in place. The prosthesis is further held in place by the normal pressure through the spine.
The Operation
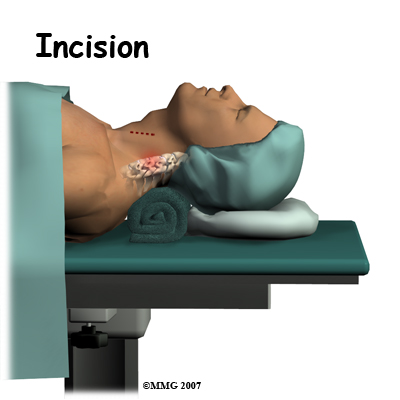
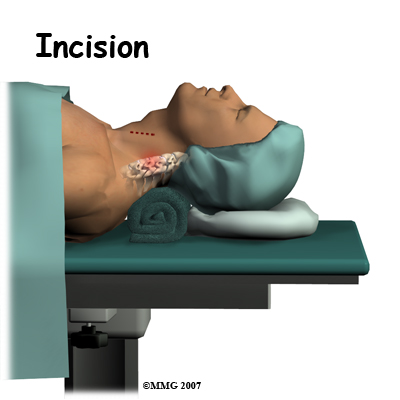
The operation is done from the anterior (front) of the body. This surgical approach is the same as that presently used for a discectomy and fusion operation. To do this, the patient is placed on his or her back. An incision is made through the skin and the thin muscles of the front of the neck. The blood vessels, the trachea (windpipe), and the esophagus are moved to the side so that the surgeon can see the front of the cervical spine. The disc that is to be replaced is identified using the fluoroscope. The fluoroscope is an x-ray machine that allows the doctor to actually see an x-ray image while doing the procedure.
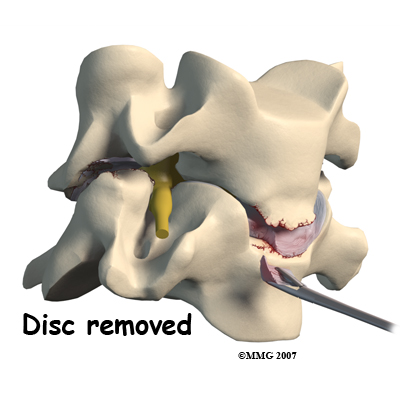
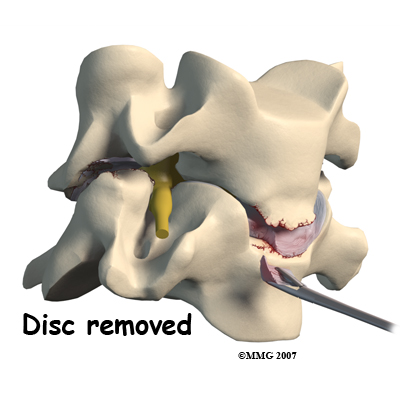
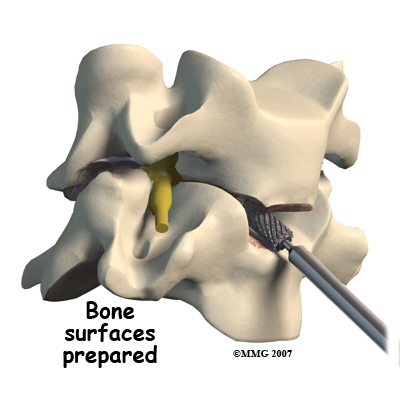
Working from the front of the spine, the spine surgeon removes a large section from the middle of the damaged disc. Next, the bones of the spine are spread apart to make more room to see and work inside the disc space. Using a surgical microscope, any remaining disc material toward the back of the disc is removed. The surgeon will also remove any disc fragments pressing against the nerve and shave off any osteophytes (bone spurs).
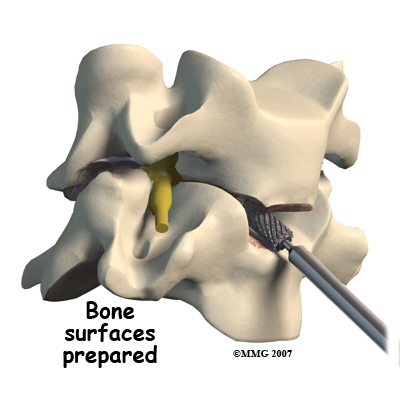
The disc space is distracted (jacked up) to its normal disc height. This step helps decompress or take pressure off the nerves. At this point, x-rays or a fluoroscope, is used to insert the artificial disc device into the prepared disc space. This allows the doctor to watch where the implant goes as it is inserted. This makes the procedure much safer and much more accurate.
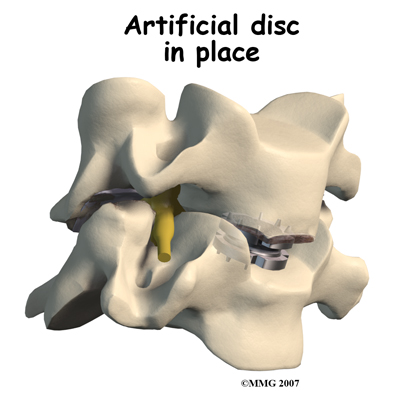
Finally, the prosthesis is tested by moving the spine in various positions. An X-ray may be taken to double check the location and fit of the new disc.
Complications
What might go wrong?
All types of spine surgery, including artificial disc replacement, have certain risks and benefits. Weigh these as you gather advice and information. Be sure to discuss the possible risks of disc replacement with your spine surgeon.
Medical complications arising from spinal surgery are rare but could include stroke, heart attack, spinal cord or spinal nerve injury, pneumonia, or possibly death.
However, information from the disc replacement operations shows a low rate of complications. There have been no reports of death, significant infection, or major neurological problems.
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications are:
- anesthesia complications
- thrombophlebitis
- infection
- blood loss
- nerve injury or paralysis
- spontaneous ankylosis (fusion)
- subsidence (sinking)
- implant failure (need for further surgery)
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia. These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat and may require additional surgery to treat the infected portion of the spine.
Blood Loss
Cervical disc replacement surgery carries risks associated with operating from the front of the spine. Blood vessels that travel near the front of the spine may be injured during anterior cervical surgery.
Nerve Injury
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to these structures can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
The nerve to the voice box is sometimes injured during surgery on the front of the neck. When doing anterior neck surgery, surgeons prefer to go through the left side of the neck where the path of the nerve to the voice box is more predictable than on the right side. During surgery, the nerve may get stretched too far when retractors are used to hold the muscles and soft tissues apart. When this happens, patients may be hoarse for a few days or weeks after surgery. In rare cases where the nerve is actually cut, patients may end up with ongoing minor problems of hoarseness, voice fatigue, or difficulty making high tones.
Spontaneous Ankylosis (fusion)
Some things can go wrong with any implant. In the case of artificial disc replacements for the cervical spine, sometimes the spine fuses itself, a process called spontaneous ankylosis. Loss of neck motion is the main side effect of this problem.
Bone may also form in the soft tissues around the vertebrae. For example, cartilage turns to bone or bone-like tissue. This process is called ossification. Ossification may not affect the implant or your final results in terms of motion or function.
Some patients are left with pain, numbness, and weakness. This can occur when there’s been incomplete neurologic decompression. In other words, there is still pressure on the spinal cord or spinal nerves.
Subsidence (sinking)
Subsidence is another possible problem. The implant actually sinks down into the vertebral body above or below it. This results in a loss of the normal disc height. Neurologic compression with neurologic symptoms can occur.
Implant Failure (need for further surgery)
Over time, wear and tear just from the physical process of motion across a bearing surface can cause tiny bits of debris to flake off the implant. The body may react to these particles with an inflammatory response that can cause pain, implant loosening, and implant failure. So far, significant inflammatory reactions have not been reported for spinal artificial disc replacements. In rare cases, the artificial disc replacement can dislocate.
After Surgery
What happens after surgery
Most people spend one or two days in the hospital. You may require an extra day or two if for some reason you’re having extra pain or unexpected difficulty. Patients generally recover quickly after the artificial disc procedure.
You should be able to get out of bed and walk within a few hours. Move carefully and comfortably, and avoid extending your neck (bending backward). You may need to wear a brace or soft collar for a short while after the operation to support your neck muscles.
As you recover in the hospital, a physical therapist may see you one or two times each day until you go home. You’ll be shown ways to move, dress, and do activities without putting extra strain on your neck. Your physical therapist will help you begin a walking program in the hospital. You are encouraged to continue the walking program when you return home.
When you leave the hospital, there are very few activity restrictions. You should be safe to sit, walk, and drive. However, you should avoid lifting items for at least four weeks. Your surgeon will probably release you to return to work in two to four weeks. If your job requires moving and lifting heavy items, you may require a longer period of recovery. Your surgeon may give you the okay to do all your activities by the sixth week after surgery.
If you spend large amounts of time in front of a computer or other machine, you may need to change the height and angle of your work surface and/or the computer. Finding a position that puts minimal stress on your neck is important. You should avoid spending hours in one position reading, sewing, or doing other handwork. The physical therapist can help you find optimal positions and advise you about ways to stretch your neck muscles.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Our Rehabilitation
What should my recovery be like?
Your surgeon may prescribe outpatient physical therapy within one to two weeks after surgery. Although the time required for recovery varies, as a guideline, plan on attending physical therapy
two to three times each week for four to six weeks.
The first few visits include treatments to calm soreness and pain from the operation. Our physical therapist may apply gentle soft-tissue treatments such as massage as well as ice and electrical stimulation to calm muscle spasm and to help take away any lasting pain.
Our physical therapist will teach you how to protect your neck. You’ll learn ways to position your neck when you sleep, sit, and drive. We'll show you ways to keep your neck safe during routine activities, such as getting in or out of bed, getting dressed, and washing your hair.
Many patients are afraid to move the head and neck for fear of damaging or dislodging the disc. Using normal motion for everyday activities will not harm your new disc in any way. Our physical therapist will help you learn how to move your neck and show you any limits necessary.
Active treatments are then used to improve flexibility, strength, and endurance. Our therapist will generally prescibe gentle stretching exercises for the neck. You’ll begin a series of strengthening exercises to help tone and control the muscles that stabilize the neck and upper back. It is also important to build strength in your arms. Our endurance exercises may include treadmill walking, swimming, or stationary biking.
When your symptoms are under control and you’re comfortable doing your exercises, your formal physical therapy sessions at Combined Therapy Specialties will end. You’ll then continue your exercises as part of a home program.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Portions of this document copyright MMG, LLC.