Introduction
Physical therapy in Asheville for Shoulder
 Welcome to Combined Therapy Specialties resource on biceps tendonitis.
Welcome to Combined Therapy Specialties resource on biceps tendonitis.
Biceps tendonitis, also called bicipital tendonitis, is inflammation of the tendon that attaches the biceps muscle to the shoulder or forearm. The tendon most commonly irritated is the one that attaches the top of the biceps muscle to the shoulder, so it is this injury that we will discuss here.
The most common cause of biceps tendonitis is overuse from certain types of work or sports activities. Biceps tendonitis may develop gradually from the effects of wear and tear, or it can happen suddenly from a direct injury. The tendon may also become inflamed in response to other problems that affect how you use the shoulder, such as rotator cuff tears, impingement in the shoulder, or shoulder instability (described below).
This guide will help you understand:
- what parts of the shoulder are affected
- the causes of biceps tendonitis
- ways to treat this problem
- what Combined Therapy Specialties approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Shoulder Pain|limit:15|heading:Hear from some of our patients who we treated for *Shoulder Pain*#
Anatomy
What parts of the shoulder are affected?
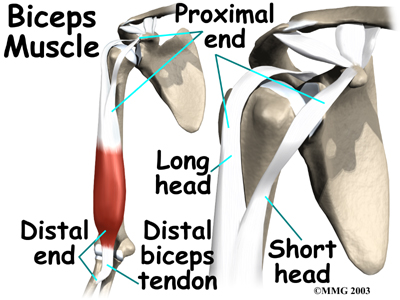
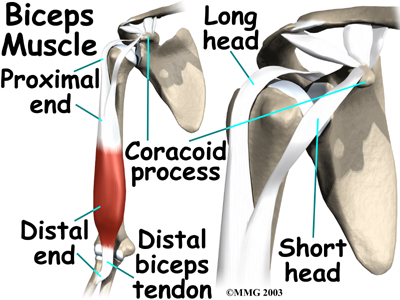
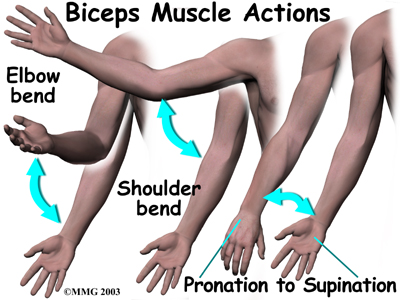
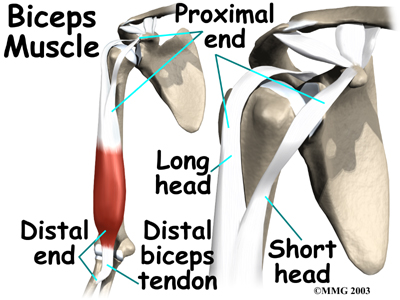
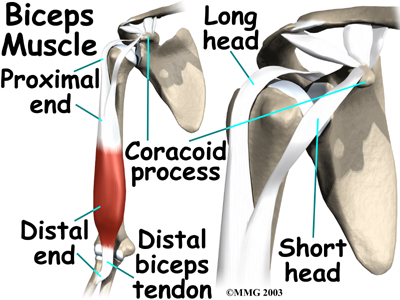
The biceps muscle goes from the shoulder to the elbow on the front of the upper arm. Two separate tendons (tendons attach muscles to bones) connect the upper part of the biceps muscle to the shoulder. The upper two tendons of the biceps are called the proximal biceps tendons, because they are closer to the top of the arm.
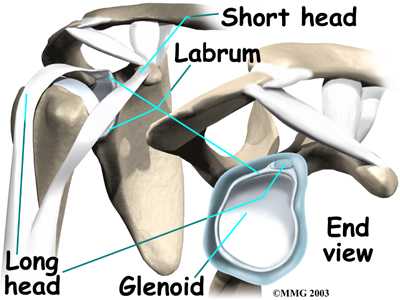
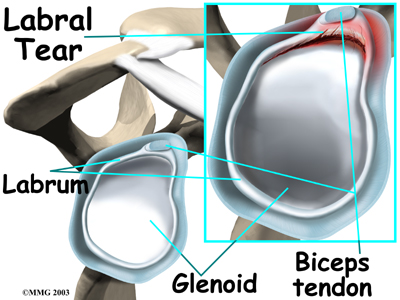
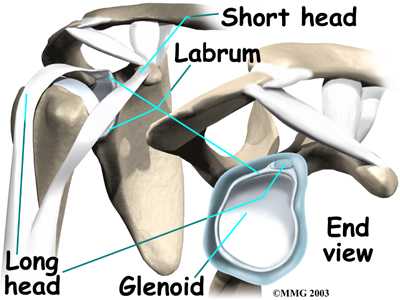
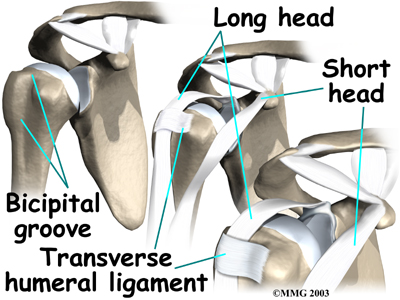
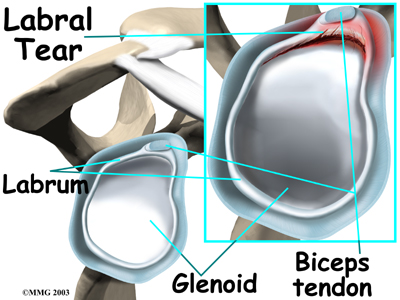
The main proximal tendon is the long head of the biceps. It connects the biceps muscle to the top of the shoulder socket, the glenoid. It also blends with the cartilage rim around the glenoid, which is called the labrum. The labrum is a rim of soft tissue that turns the flat surface of the glenoid into a deeper socket. This arrangement improves the fit of the ball of the humerus (humeral head) in to the socket.
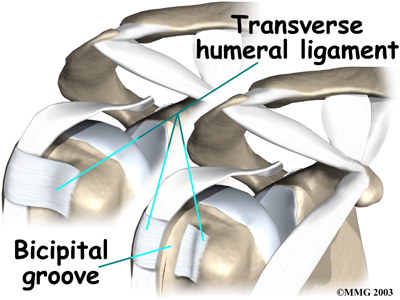
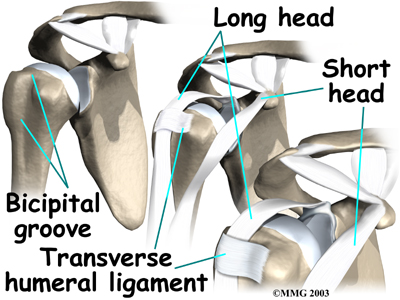
Beginning at the top of the glenoid, the tendon of the long head of the biceps runs in front of the humeral head. The tendon passes within the bicipital groove of the humerus and is held in place by the transverse humeral ligament. This design of the anatomy keeps the humeral head from sliding too far up or forward within the glenoid.
The short head of the biceps connects onto the coracoid process of the scapula (shoulder blade). The coracoid process is a small bony knob just in from the front of the shoulder. The lower biceps tendon is called the distal biceps tendon. The word distal means the tendon is further down the arm. The lower part of the biceps muscle connects to the forearm by this tendon. The muscles forming the short and long heads of the biceps stay separate until just above the elbow, where they unite and connect to the distal biceps tendon.
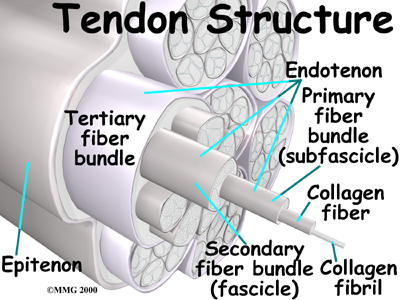
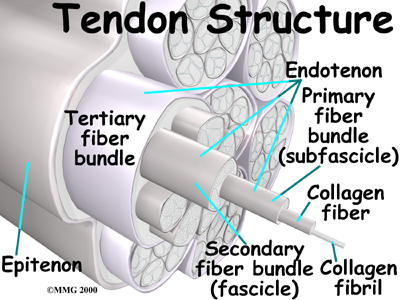
Tendons are made up of strands of a material called collagen. The collagen strands are lined up in bundles next to each other. Due to the collagen strands in tendons lining up, tendons have high tensile strength. This means they can withstand high forces that pull on both ends of the tendon. When muscles work, they pull on one end of the tendon. The other end of the tendon pulls on the bone, causing the bone to move.
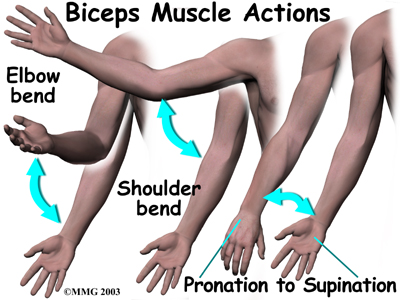
Contracting the biceps muscle can bend the elbow upward. The biceps can also help move the shoulder by lifting the arm up in front of the body, a movement called shoulder flexion. The biceps muscle can also rotate, or twist, the forearm in a way that points the palm of the hand up. This movement is called supination, which positions the hand as if you were holding a tray.
Related Document: Combined Therapy Specialties Guide to Shoulder Anatomy
Shoulder Anatomy Introduction
Causes
Why is my biceps tendon inflamed?
Continuous or repetitive shoulder actions can cause overuse of the biceps tendon. Damaged cells within the tendon don't have time to recuperate or the cells are unable to repair themselves, leading to tendonitis. This is common in sport or work activities that require frequent and repeated use of the arm, especially when the arm motions are performed overhead. Athletes who throw, swim, or swing a racquet or club are at greatest risk.
Years of shoulder wear and tear can also cause the biceps tendon to become painful. Examination of the tissues in cases of wear and tear commonly shows signs of degeneration. Degeneration in a tendon causes a loss of the normal arrangement of the collagen fibers that join together to form the tendon. Some of the individual strands of the tendon become jumbled due to the degeneration, and other fibers break which both cause the tendon to lose strength. When this happens in the biceps tendon a rupture of the tendon may occur.
Biceps tendonitis can also happen from a direct injury, such as a fall onto the top of the shoulder. A torn transverse humeral ligament can also lead to biceps tendonitis. As mentioned earlier, the transverse humeral ligament holds the biceps tendon within the bicipital groove near the top of the humerus. If this ligament is torn, the biceps tendon is free to jump or slip out of the groove, irritating and eventually inflaming the biceps tendon.
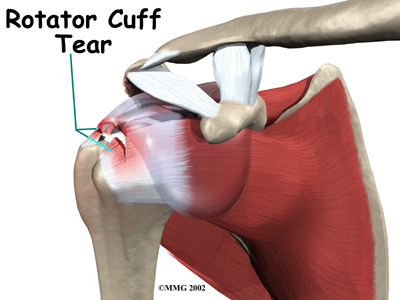
Biceps tendonitis sometimes occurs in response to other shoulder problems which affect the way you use your shoulder, including rotator cuff tears, shoulder impingement, and shoulder instability.
Aging adults with rotator cuff tears commonly end up with biceps tendonitis. When the rotator cuff is torn, the humeral head is free to move too far up and forward in the shoulder socket and can impact the biceps tendon. The damage may begin to weaken the biceps tendon and cause it to become inflamed.
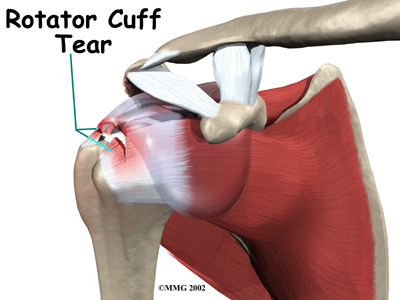
Related Document: Combined Therapy Specialties Guide to Rotator Cuff Tears
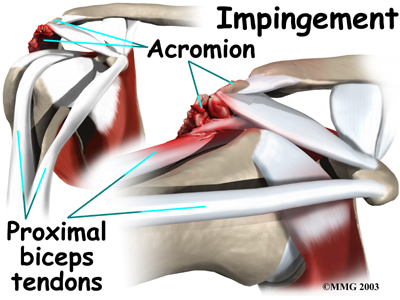
In shoulder impingement, the soft tissues between the humeral head and the top of the shoulder blade (acromion) get pinched or squeezed with certain arm movements. This pain affects the way you move your shoulder, and often the biceps muscle is overused to compensate or is physically pinched which causes it to become inflamed.
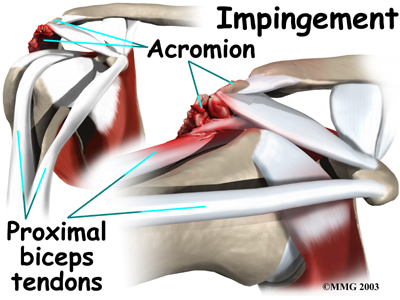
Related Document: Combined Therapy Specialties Guide to Shoulder Impingement
Conditions that allow too much movement of the ball within the socket create shoulder instability. When extreme shoulder motions are frequently repeated, such as with throwing or swimming, the soft tissues supporting the ball and socket can eventually get stretched out. In other cases, the shoulder may become unstable from a traumatic event where the joint subluxes or has been dislocated. Again, this instability then affects the way you use your shoulder, and the biceps muscle can be overused, leading to secondary pain and inflammation in the tendon.
Related Document: Combined Therapy Specialties Guide to Shoulder Instability
With chronic instability of the shoulder the labrum (the cartilage rim that deepens the glenoid, or shoulder socket) may begin to pull away from its attachment to the glenoid, sometimes near where the biceps tendon attaches. A shoulder dislocation can also cause the labrum to tear. When the labrum is torn, the humeral head may begin to slip up and forward within the socket. Once again, the biomechanics of the shoulder joint are affected and the biceps tendon often becomes inflamed as a result.
Related Document: Combined Therapy Specialties Guide to Labral Tears
Symptoms
What does biceps tendonitis feel like?
Patients generally report the feeling of a deep ache directly in the front and top of the shoulder. This area will also be sensitive to touch, especially in comparison to the other side. The aching may spread down into the main part of the biceps muscle. Pain is usually made worse with overhead activities. Resting the shoulder generally eases pain.
In addition, the arm may feel weak with attempts to bend the elbow or when twisting the forearm into supination (palm up). A catching or slipping sensation felt near the top of the biceps muscle may suggest a tear of the transverse humeral ligament.

Diagnosis
How can my health care professional be sure I have biceps tendonitis?
The history and physical examination are probably the most important tools that health care professionals, including your physical therapist at Combined Therapy Specialties, will use to diagnose this problem. Your therapist will want to know exactly where your pain is, when it started, and what activities ease or aggravate your symptoms. If you are involved in sport, your training history including any increases in volume of activity or change in equipment will also be important for us to inquire about.
Next your physical therapist will physically examine your shoulder. First they will look at the way you hold your shoulder with your natural posture in sitting and standing. The positioning of your upper back and neck can also affect the functioning of your shoulder so they will also observe this. Your therapist will touch, or palpate, around your painful area as well as other areas on your shoulder to help differentiate that it is truly your biceps tendon causing the pain. They will compare the tenderness you feel from side to side as often a normal biceps tendon can have some tenderness when palpated in the groove. Your problem side will feel more tender when touched than your normal side.
Next your physical therapist will ask you to move your arm in different directions to determine how much range of motion you can achieve on your own, to see how you move your shoulder, and also to determine how much strength you have in your shoulder.
They will then ask you to relax your arm while they move your arm themselves. It is imperative that you try to relax as much as possible during this motion and do not help with your muscles so that your therapist can determine how much discomfort you are in if you are not activating your own muscles. Your physical therapist will then assess the resisted motions of your shoulder, including the strength of the rotator cuff and the biceps tendon itself. With biceps tendonitis there is not always an obvious decrease in strength of the biceps muscle itself. Pain when functionally using the muscle and associated tendon is a more common symptom than an obvious decrease in strength. However an associated decline in rotator cuff strength is quite common when the biceps tendon is irritated.
The next part of the physical assessment will include your physical therapist performing some special tests to confirm the diagnosis of biceps tendonitis. Other special tests can determine if nearby structures are causing problems, such as a tear in the labrum, a tear in the transverse humeral ligament, or if there are impingement or rotator cuff problems.
Combined Therapy Specialties provides services for physical therapy in Asheville
Physician’s Review
If biceps tendonitis is suspected X-rays are generally not needed right away. If the shoulder doesn’t get better with treatment, however, they may be ordered. An X-ray can show if there are bone spurs or calcium deposits near the tendon. X-rays can also show if there are other problems, such as a small fracture. Plain X-rays do not show soft tissues like tendons and will not show a biceps tendonitis specifically.
When the shoulder isn't responding to treatment, a magnetic resonance imaging (MRI) scan may also be ordered. An MRI is a special imaging test that uses magnetic waves to create pictures of the shoulder in slices. This test can tell if there are problems in the rotator cuff or labrum, and can also show inflammation around the biceps tendon.
In rare instances, an injection of cortisone may be used to try to control pain. Cortisone is a very powerful steroid. However, cortisone is used very sparingly because it can weaken the biceps tendon, and possibly cause it to rupture.
Arthroscopy is an invasive way to evaluate shoulder pain that isn't going away. It is not used as an initial investigative exam for biceps tendonitis. It may be used, however, for ongoing shoulder problems where a cause has not been identified in an X-ray or MRI scan, or for shoulders that are not responding to conservative treatment. An arthroscope is a thin instrument that has a tiny camera on the end, which the surgeon uses to see inside the joint. It can show if there are problems with the rotator cuff, the labrum, or the portion of the biceps tendon that is inside the shoulder joint.
Treatment
What treatment options are available?
Whenever possible, doctors treat biceps tendonitis without surgery. Anti-inflammatory medicine may be prescribed to ease the pain and to help patients return to normal activity. These medications include common over-the-counter drugs such as ibuprofen.
A crucial part of non-conservative treatment for biceps tendonitis is physical therapy treatment.
Physical therapy at Combined Therapy Specialties can be extremely effective in treating biceps tendonitis.
Our initial aim with physical therapy treatment is to decrease the pain and inflammation around the tendon. Your physical therapist may use electrical modalities for this purpose such as ultrasound or electrical current. Heat and/or ice can also be very useful in decreasing pain and inflammation so your therapist will encourage you to use heat or ice frequently at home; they can advise you on whether heat or ice is best for your particular injury. Your physical therapist may also use massage around the shoulder, into the biceps muscle, and up into your neck area to ease your discomfort and assist with the associated inflammation.
A period of relative rest will also make a notable improvement in your shoulder pain. Relative rest indicates that you do not have to stop doing all activity, but rather that you stop or limit the amount of those activities that aggravate your shoulder. Resting your shoulder is crucial, along with simultaneous physical therapy treatment, to calm the pain and inflammation associated with your injury.
Once the pain and inflammation are under control, your physical therapy treatment will focus on regaining the range of motion, strength, and coordination in your shoulder. Your physical therapist at Combined Therapy Specialties will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of a home exercise program.
It is easiest to move the shoulder joint through its full range of motion if it is done passively, which means that you don’t use the muscles on your injured side to lift the shoulder. Your therapist may ask you to use a pole or a pulley in order to lift your arm up overhead or behind your back. If you do not maintain the motion in your shoulder by at least passively moving it through its full range of motion, it is easy for a frozen shoulder to develop. With a frozen shoulder the tissues in the shoulder actually shorten and tighten up such that anatomically the full shoulder range is no longer possible. All passive range of motion exercises prescribed should be done within the limits of pain, however there may be a mild discomfort as you reach the end of your range of motion, and this is normal. This mild discomfort is not detrimental to your progress so long as the pain remains at a very mild level. In some cases your physical therapist themselves may move your shoulder for you in order to stretch it; again, this is considered passive motion. An upper body bike may also be useful in the early stages of rehabilitation to improve range of motion and encourage coordinated movement of the entire upper limb, as long as it can be used without causing more than mild discomfort.
A crucial component to any shoulder rehabilitation program is the ability for you to regain what is called ‘proprioceptive control’ of your shoulder joint. Proprioception is the ability to know where your body is without looking at it. For example, normally each time you reach overhead with your hand, your mind does not consciously have to think about doing the action, yet all of the muscles of the shoulder (and elbow, wrist, and upper back) coordinate the action just right so you can perform the movement without any discomfort or pinching. When you have pain in a joint, or the tissues of the joint have been injured, your proprioception declines. Any period of decreased mobility of the joint will also add to this decline. If the proprioceptive control of your shoulder is poor then the ability to use your shoulder naturally in all ranges of movement without causing any pain or pinching, or unnecessary motion, declines, and your shoulder is at risk of increased wear and tear, and developing another injury. The biceps tendon is very susceptible to feeling the effects of poor shoulder proprioception, and inflammation in the tendon can easily occur.
The joint between your shoulder blade and your thoracic spine (called the scapulothoracic joint) is particularly important to the overall proprioceptive control of the shoulder joint. The outer edge of the shoulder blade actually creates the socket of the shoulder joint. Together, the scapulothoracic joint and the shoulder joint itself (including the rotator cuff muscles) create the complete shoulder girdle; the entire shoulder girdle must operate together for normal shoulder motion. Controlled shoulder girdle motion along with adequate rotator cuff strength keeps the ball of the shoulder joint properly centered in the socket of the joint and avoids any pain or undesired motion of the joint. This centered position of the ball in the socket also keeps the ball of the shoulder joint from drifting forward and pressing on the biceps tendon, which causes unnecessary pressure and irritation. The control and strength of the scapulothoracic joint is particularly essential when using your limb is near or above shoulder height and especially during rapid or repetitive arm movements such as throwing.
For this reason, your physical therapist will teach you how to properly control your shoulder girdle during your rehabilitation exercises but will also educate you on transferring this control to your everyday activities. Again, this will prevent excessive wear and tear on your shoulder joint even during the repetition of normal everyday tasks. Adequate control of the shoulder girdle is important to establish even before beginning any strengthening of the biceps muscle or the rotator cuff tendons.
In order gain the appropriate balanced strength in your rotator cuff muscles of the shoulder joint, as well as to address any biceps muscle weakness that may have developed your physical therapist at Combined Therapy Specialties will also prescribe strength specific exercises. Adequate strength in the rotator cuff can relieve pressure on the biceps tendon. Strength exercises may involve using light weights or Theraband to add resistance for your upper limb. As stressed above, an irritable biceps tendon can easily be made more irritable if your control and technique while performing strengthening exercises is poor, so your therapist will repeatedly focus on proper shoulder proprioception and exercise technique while you perform your exercises. Adequate strength and endurance in the rotator cuff muscles throughout a variety of ranges of motion, including above shoulder height, is needed to ensure full functioning of the shoulder.
As you improve with being able to control the shoulder girdle and as your strength improves your physical therapist will introduce more difficult dynamic exercises for your shoulder. These may include exercises that simulate your daily tasks, or if you are a high-level athlete or particpate in recreational sport, those shoulder motions that simulate your sport. Simple proprioceptive exercises might include activities such as rolling a ball on a surface with your hand, holding a weight up overhead while moving your shoulder, or even doing push-ups on an unstable surface. Advanced exercises may include activities such as ball throwing, catching overhead, or a simulated swimming stroke or overhead volleyball spike.
Finally, as part of your shoulder rehabilitation, your physical therapist will also remind you about maintaining good shoulder posture at all times even when just sitting or using your upper limb in activities below shoulder height, such as working on the computer. Rounded shoulders in any position crowds the shoulder joint and can lead to shoulder impingement, more pressure on the biceps tendon, poor recovery from your injury, or even the development of a new episode of shoulder pain. Simple changes in the way you sit or stand and how you use your shoulder, neck and thoracic spine throughout the day can ease your pain and help you avoid further problems.
In addition to rehabilitating your shoulder joint itself, at Combined Therapy Specialties we highly recommend maintaining the rest of your body’s fitness with regular exercise even while you recover from the biceps tendonitis in your shoulder. Cardiovascular fitness can be maintained with lower extremity fitness activities such as walking or using a stationary bike or stepper machine. None of these exercises should cause discomfort to your shoulder; if they do, discuss modifying the activity with your physical therapist.
You will notice improvements in the functioning of your shoulder even after just a few treatments with your physical therapist at Combined Therapy Specialties. If, however, your shoulder joint is not recovering as your % physiotherapist% would expect it should, or if your pain becomes unmanageable, your physical therapist will suggest that you return to your doctor and/or see an Orthopaedic Surgeon. More radical treatment measures, such as surgery, may be needed in your case to deal with the problem.
Combined Therapy Specialties provides services for physical therapy in Asheville
Surgery
Patients who are improving with conservative treatments do not typically require surgery. Surgery may be recommended, however, if the problem doesn't go away or when there are other shoulder problems present besides the biceps tendonitis.
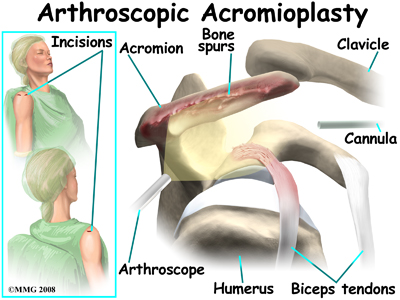 The most common surgery for bicipital tendonitis is acromioplasty, especially when the underlying problem is shoulder impingement. This procedure involves removing the front portion of the acromion, which is the bony ledge formed where the scapula meets the top of the shoulder joint. By removing a small portion of the acromion, more space is created between the acromion and the humeral head. This takes pressure off the soft tissues in between, including the biceps tendon.
The most common surgery for bicipital tendonitis is acromioplasty, especially when the underlying problem is shoulder impingement. This procedure involves removing the front portion of the acromion, which is the bony ledge formed where the scapula meets the top of the shoulder joint. By removing a small portion of the acromion, more space is created between the acromion and the humeral head. This takes pressure off the soft tissues in between, including the biceps tendon.
Today, acromioplasty is usually done using an arthroscope. An arthroscope is a slender tool with a tiny TV camera on the end. It lets the surgeon work inside the joint through a very small incision. This may result in less damage to the normal tissues surrounding the joint, leading to faster healing and recovery.
To perform the acromioplasty using the arthroscope, several small incisions are made to insert the arthroscope and other special instruments needed to complete the procedure. These incisions are small, usually about one-quarter inch long. It may be necessary to make three or four incisions around the shoulder to allow the arthroscope to be moved to different locations and to view different areas of the shoulder.
A small plastic or metal tube is inserted into the shoulder and connected with sterile plastic tubing to a special pump. Another small tube allows the fluid to be removed from the joint. This pump continuously fills the shoulder joint with sterile saline (salt water) fluid.
This constant flow of fluid through the joint inflates the joint and washes any blood and debris from the joint as the surgery is performed.
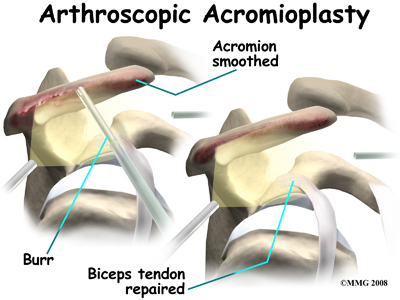 There are many small instruments that have been specially designed to perform surgery in the joint. Some of these instruments are used to remove torn and degenerative tissue. Some of these instruments nibble away bits of tissue and then vacuum them out of the joint. Others are designed to burr away and then vacuum up bone spurs that are rubbing on the tendons of the shoulder under the acromion.
There are many small instruments that have been specially designed to perform surgery in the joint. Some of these instruments are used to remove torn and degenerative tissue. Some of these instruments nibble away bits of tissue and then vacuum them out of the joint. Others are designed to burr away and then vacuum up bone spurs that are rubbing on the tendons of the shoulder under the acromion.
If necessary, the acromioplasty can also be performed using the older, open method. The open method requires an incision in the skin over the shoulder joint. Working through the incision, the surgeon locates the deltoid muscle on the outer part of the shoulder. Splitting the front section of this muscle gives the surgeon a better view of the acromion. Some surgeons also detach the deltoid muscle where it connects on the front of the acromion.
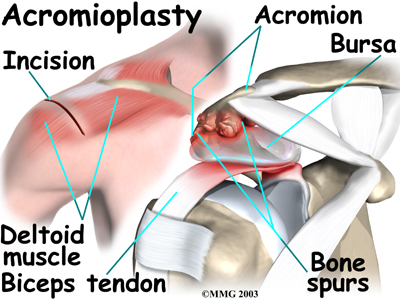
The bursa sac that lies just under the acromion is removed. Next, a surgical tool is used to cut a small portion off the front of the acromion. The ligament arcing from the acromion to the corocoid process (the coracoacromial ligament) may also be removed.
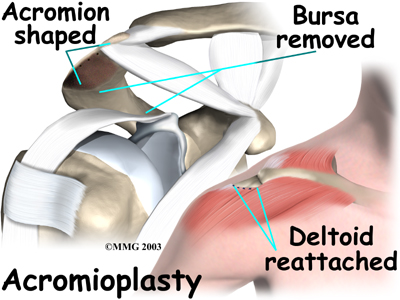 The surgeon then shaves the undersurface of the acromion to remove any bone spurs. A file is used to smooth the edge of the acromion. Next, a series of small holes are drilled into the remaining acromion. These holes are used to reattach the deltoid muscle to the acromion.
The surgeon then shaves the undersurface of the acromion to remove any bone spurs. A file is used to smooth the edge of the acromion. Next, a series of small holes are drilled into the remaining acromion. These holes are used to reattach the deltoid muscle to the acromion.
While inside the joint the surgeon inspects the rotator cuff muscle to see if any tears are present. Next the entire area is irrigated to wash away small particles of bone. Finally, the free end of the deltoid muscle is sutured back to the ridge of the acromion using the drill holes made earlier.
If upon internal examination the biceps tendon is severely degenerated, the surgeon may perform a biceps tenodesis (described next). The surgeon completes the procedure by closing the incision with sutures.
Biceps tenodesis is a method of reattaching the top end of the biceps tendon to a new location. Studies show that the long-term results of this form of surgery are not satisfactory for patients with simple biceps tendonitis. However, tenodesis may be needed when the biceps tendon is severely degenerated or when shoulder reconstruction for other problems is needed.
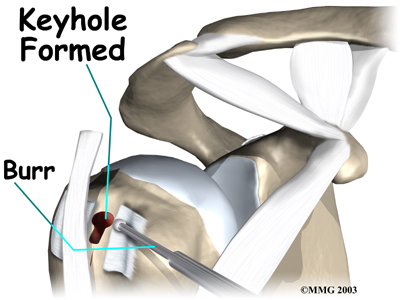
A common method of performing a biceps tenodesis is called the keyhole technique. The keyhole describes the shape of a small hole made by the surgeon in the humerus. The end of the tendon is slid into the top of the keyhole and pulled down to anchor it in place.
This surgery can be done using the arthroscope. The tenodesis procedure is usually combined with other procedures such as acromioplasty which was described above. If this is the case, the surgeon will simply continue using the arthroscope to do the tenodesis procedure if possible. Again, the advantage of using the arthroscope is that less normal tissue is damaged and this may result in faster healing and recovery.
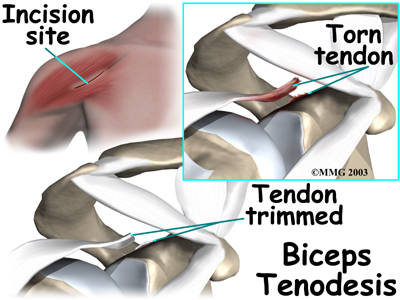 If the procedure is performed using the open method, however, the surgeon begins by making an incision on the front of the shoulder, just above the axilla (armpit). The overlying muscles are separated so the surgeon can locate the top of the biceps tendon. The end of the biceps tendon is removed from its attachment at the top of the glenoid. The tendon is prepared by cutting away frayed and degenerated tissue.
If the procedure is performed using the open method, however, the surgeon begins by making an incision on the front of the shoulder, just above the axilla (armpit). The overlying muscles are separated so the surgeon can locate the top of the biceps tendon. The end of the biceps tendon is removed from its attachment at the top of the glenoid. The tendon is prepared by cutting away frayed and degenerated tissue.
The transverse humeral ligament is split, exposing the bicipital groove and an incision is made along the floor of the bicipital groove.
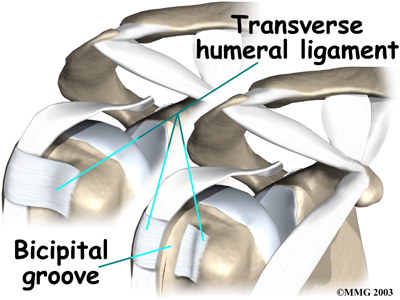
The bleeding from the incision encourages scar tissue to form that will help anchor the repaired tendon in place.
A burr is used to form a keyhole-shaped cavity within the bicipital groove. The top of the cavity is round. The bottom is the slot of the keyhole, which is made the same width as the biceps tendon.
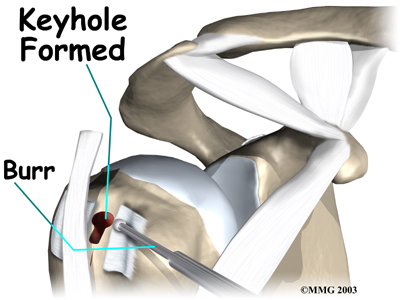
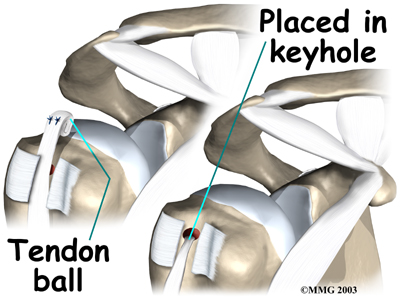
The surgeon rolls the top end of the biceps tendon into a ball. Sutures are used to form and hold the ball in place. The elbow is then bent, taking tension off the biceps muscle and tendon. Next the surgeon pushes the tendon ball into the top part of the keyhole.
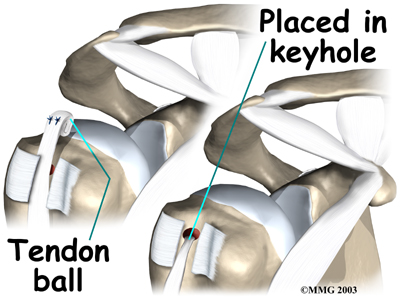
As the elbow is gradually straightened, the ball is pulled firmly into the narrow slot in the lower end of the keyhole, which anchors the tendon.
Post Surgical Rehabilitation
Some surgeons recommend their patients start a gentle range-of-motion program immediately after surgery. If this is the case, your physical therapy at Combined Therapy Specialties can begin immediately. Other surgeons prefer to wait to allow the tissues to heal for a short time before any stress is added to them, even just gentle exercise. In this case, once your surgeon allows it, you will begin your rehabilitation at Combined Therapy Specialties.
Arthroscopic procedures that simply clean out the joint, such as acromioplasty (without a tenodesis,) progress very quickly with regards to rehabilitation and the shoulder requires minimal precautions. If you have had a tenodesis, however, whether it was done arthroscopically or with an open incision, you will need to be cautious with several shoulder activities and will need to avoid heavy arm activity for three to four weeks. This will allow the new site of the attached biceps tendon to heal adequately before it is stressed. You will likely need therapy at Combined Therapy Specialties for 6-8 weeks, but you will need to continue to do your home exercise program for 3-4 months or possibly longer to regain full functioning of your shoulder.
Your may be required to wear a sling to support and protect the shoulder for a few days after surgery whether you have had an open or arthroscopic procedure. Your surgeon or physical therapist will advise you when it is safe to stop using the sling; it is rarely used for long. If there is pain when you are not using the sling due to the weight of the shoulder, it can be protected from the hanging weight of the arm by slipping your thumb into the waist of your pants, or jeans pocket.
Good posture and adequate shoulder proprioception (discussed in detail above under non-surgical rehabilitation) is also crucial to post-surgical rehabilitation. Crowding the shoulder joint with slouched posturing or poor shoulder girdle control will add pressure to the biceps tendon will lead to ongoing inflammation, pain, and wear and tear in the shoulder joint. For this reason, posture and proprioception will be one of the first issues that your physical therapist at Combined Therapy Specialties addresses with you post-surgically.
During the initial stage of treatment at Combined Therapy Specialties after surgery your physical therapist may use ice and electrical modalities to help control pain and swelling from the surgery. They may also use massage and gentle mobilizations of your joint to ease any muscle spasm and pain.
Next your physical therapist will prescribe range-of-motion exercises for your shoulder, elbow, and hand. Your range of motion may seem quite limited initially, especially in the end ranges of motion such as reaching over-shoulder height. Reaching behind your back should be avoided initially as this puts the maximum amount of stress on the biceps tendon. Getting the shoulder moving as soon as possible is important, however, this must be balanced with the need to protect the healing tissues. Your physical therapist will guide you through the appropriate exercises at the appropriate time and ensure that you are advancing your exercises as quickly as you can without putting unnecessary stress on the surgical site.
Range of motion exercises will first be done passively, which means you will use either your other arm to lift your surgical arm, or a pulley or pole to do the lifting rather than the muscles of your surgical shoulder. Your physical therapist may also do some passive stretching of your joint in the early stages of your rehabilitation. Early passive movement of your shoulder joint into its ranges of motions is crucial to full recovery of your shoulder joint after surgery. Proper posturing during the passive range of motion exercises will help the shoulder joint move most naturally and avoid any secondary pain and impingement. As you are able, your physical therapist will advance your exercises so that you actively use your own muscle power to take your shoulder into the different ranges of motion. They will also inform you when it is safe to put more stress on the biceps tendon such as reaching high up overhead or behind your back.
Strengthening your shoulder after surgery will begin very early on but with only light isometric strengthening exercises. Isometric strengthening exercises involve tightening your muscles without actually moving the associated joint. Isometric exercises work the muscles without straining the injured or painful tissues. Your physical therapist will teach you how to use your other hand or the wall for resistance while you flex and tighten your muscles, creating an isometric contraction of the shoulder muscles. Your shoulder joint should not move during isometric exercises, hence why they can be done early on post-surgically and do not harm the healing tissue. Pain should be used as a strict limit during these exercises.
You may begin early on to do isometric biceps strengthening, but your physical therapist will ensure that it is done with your elbow bent and with your shoulder in line with your body to protect the tenodesis site. Forceful tightening of this muscle even isometrically will not be encouraged initially, but as time heals the tissue, your therapist will allow you to progress this exercise so you are putting more stress through the biceps and the surgical site.
As soon as it is safe your physical therapist will then progress your exercises so that you are strengthening the muscles through their available ranges of motion rather than isometrically, including the biceps muscle. Depending on your progression, resisted exercises for the biceps may not be added even until one month after surgery. Resisted exercises may involve using light-weights or Theraband for your upper limb. Adequate strength and endurance in the rotator cuff muscles throughout a variety of ranges of motion, including over shoulder height, is needed to ensure full functioning of the shoulder. Again, as mentioned above, adequate shoulder proprioception is crucial while strengthening the shoulder, so significant time during your rehabilitation sessions at Combined Therapy Specialties may be spent perfecting your shoulder girdle control.
As your shoulder strength improves, your physical therapist will start to introduce exercises that simulate the activities you regularly participate in, whether that be sporting activities, or work-related activities such as lifting or prolonged desk work. As you improve, you will no longer need to regularly attend physical therapy at Combined Therapy Specialties. Eventually your physical therapist will become more of a resource, while your home exercise program will be your main form of therapy. Your physical therapist will still be crucial, however, to guiding your progress and ensuring that you don’t do too much, too quickly and that the shoulder and its function recovers as it should post-surgically. As usual, your physical therapist will keep a close watch on your progression of improvement after surgery, and if you are not improving as we would expect, or your pain is not well controlled during your rehabilitation, we will ask you to return to your surgeon for follow-up to ensure there are no complicating factors impeding your recovery.
Combined Therapy Specialties provides services for physical therapy in Asheville
Portions of this document copyright MMG, LLC.
 Welcome to Combined Therapy Specialties resource on biceps tendonitis.
Welcome to Combined Therapy Specialties resource on biceps tendonitis.







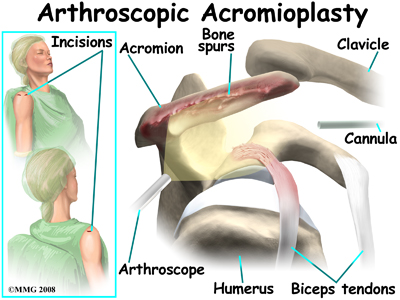 The most common surgery for bicipital tendonitis is acromioplasty, especially when the underlying problem is shoulder impingement. This procedure involves removing the front portion of the acromion, which is the bony ledge formed where the scapula meets the top of the shoulder joint. By removing a small portion of the acromion, more space is created between the acromion and the humeral head. This takes pressure off the soft tissues in between, including the biceps tendon.
The most common surgery for bicipital tendonitis is acromioplasty, especially when the underlying problem is shoulder impingement. This procedure involves removing the front portion of the acromion, which is the bony ledge formed where the scapula meets the top of the shoulder joint. By removing a small portion of the acromion, more space is created between the acromion and the humeral head. This takes pressure off the soft tissues in between, including the biceps tendon.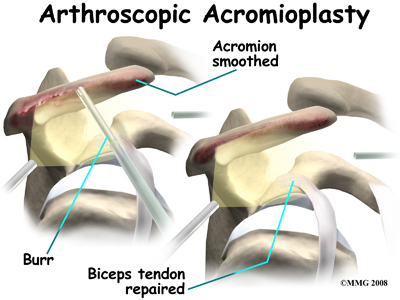 There are many small instruments that have been specially designed to perform surgery in the joint. Some of these instruments are used to remove torn and degenerative tissue. Some of these instruments nibble away bits of tissue and then vacuum them out of the joint. Others are designed to burr away and then vacuum up bone spurs that are rubbing on the tendons of the shoulder under the acromion.
There are many small instruments that have been specially designed to perform surgery in the joint. Some of these instruments are used to remove torn and degenerative tissue. Some of these instruments nibble away bits of tissue and then vacuum them out of the joint. Others are designed to burr away and then vacuum up bone spurs that are rubbing on the tendons of the shoulder under the acromion. 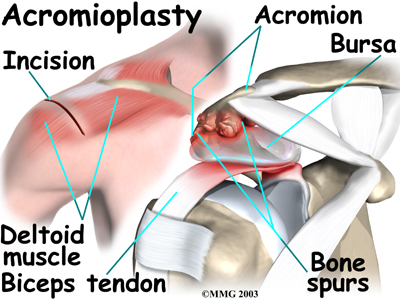
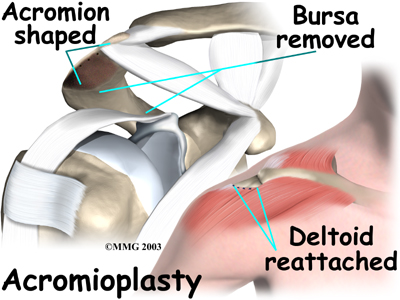 The surgeon then shaves the undersurface of the acromion to remove any bone spurs. A file is used to smooth the edge of the acromion. Next, a series of small holes are drilled into the remaining acromion. These holes are used to reattach the deltoid muscle to the acromion.
The surgeon then shaves the undersurface of the acromion to remove any bone spurs. A file is used to smooth the edge of the acromion. Next, a series of small holes are drilled into the remaining acromion. These holes are used to reattach the deltoid muscle to the acromion.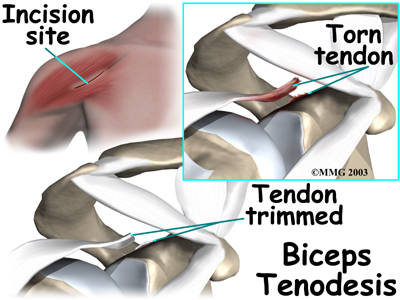 If the procedure is performed using the open method, however, the surgeon begins by making an incision on the front of the shoulder, just above the axilla (armpit). The overlying muscles are separated so the surgeon can locate the top of the biceps tendon. The end of the biceps tendon is removed from its attachment at the top of the glenoid. The tendon is prepared by cutting away frayed and degenerated tissue.
If the procedure is performed using the open method, however, the surgeon begins by making an incision on the front of the shoulder, just above the axilla (armpit). The overlying muscles are separated so the surgeon can locate the top of the biceps tendon. The end of the biceps tendon is removed from its attachment at the top of the glenoid. The tendon is prepared by cutting away frayed and degenerated tissue.