Introduction
Physical therapy in Asheville for Lower Back Issues
Welcome to Combined Therapy Specialties resource about Spondyloarthropathies.

There are many different types of rheumatological diseases that affect the spine. A rheumatological disease is a problem that affects the entire body as a whole, rather than just one joint, such as the relatively well-known rheumatoid arthritis. When a rheumatological disease affects the spine, the resulting conditon is called a spondyloarthropathy. The term is made up of the Greek words: "Spondylo" meaning "vertebra," "arthro" meaning "joint," and "pathos" meaning "disease."
The most common diseases in the spondyloarthropathies category include:
- Ankylosing Spondylitis (AS)
- Psoriatic Arthritis (PsA)
- Reactive Arthritis (ReA)
- Enteropathic Arthritis (EA)
- Rheumatoid Arthritis (RA)
This guide will help you understand:
- which parts of the spine are affected
- what causes these diseases
- what the most common symptoms are
- how health care professionals diagnose the problem
- what treatment options are available
- Combined Therapy Specialties approach to rehabilitation
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
This group of diseases cause damage by creating inflammation that attacks the connective tissues of the body. Connective tissue makes up many structures in the body including bones, tendons, ligaments, cartilage, blood and lymphatic tissue. In most cases, the cause of these diseases is unknown. There is increasing evidence that the underlying cause may be a combination of genetics and infection. A person born with certain genes may react differently to certain types of infections. Once that person is exposed to certain infections, the body responds by defending itself. The way the body defends itself against infection is through an inflammatory response. This is normal. What is not normal is that long after the infection is gone, the inflammation continues. This chronic inflammation causes damage to many of the connective tissue structures in the body often causing pain and dysfunction.
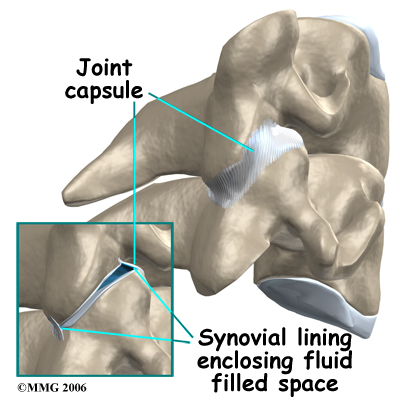
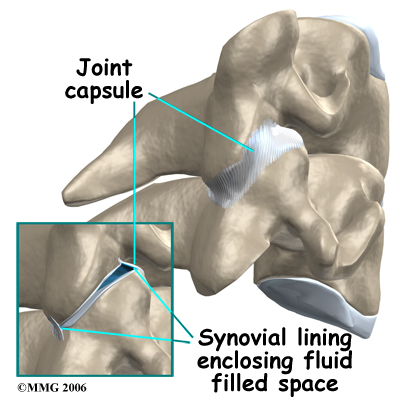
As mentioned above, there are several rheumatological diseases that can affect the spine. One of the most common rheumatological diseases is rheumatoid arthritis (RA). RA primarily attacks the synovial joints and unfortunately a lot of the joints in the body are synovial joints, such as the knee, hip, shoulder, and knuckle joints. Synovial joints are flexible connections that require the two bones can move against one another. The ends of the bones are covered with articular cartilage. Articular cartilage is a white, shiny material that is very slippery and has a limited blood supply. It provides shock absorption and allows the bones to glide easily against one another. The synovial joint is completely enclosed by a joint capsule made up of tough connective tissue on the outside and a thin layer of tissue on the inside called the synovial lining. Inside the joint there is a small amount of fluid called synovial fluid. The synovial fluid brings nutrients to the articular cartilage as it lubricates the joint.
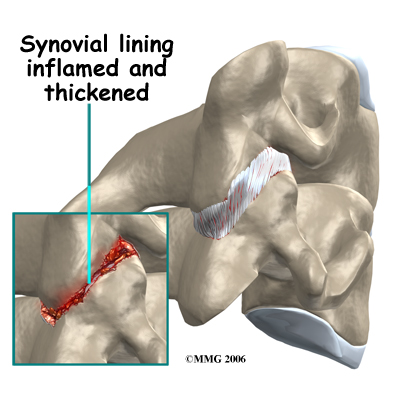
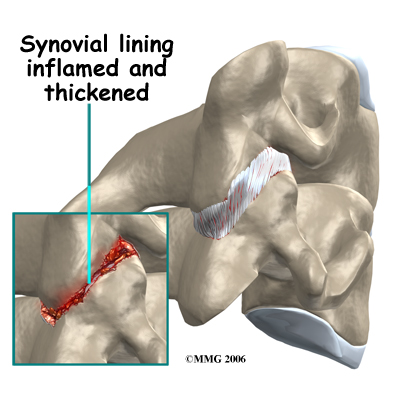
In RA, the synovial lining of the joint is affected. The normally thin tissue of the synovial lining becomes inflamed and thickened. This material begins to produce inflammatory chemicals that damage the articular cartilage and bone underneath. The joint is slowly destroyed until bone rubs against bone. In the spine, there are synovial joints between each vertebra and between the skull and the first cervical vertebra. With so many synovial joints in the spine, it is obvious why patients with RA often feel the disease there, and why it is categorized as a spondyloarthropathy.
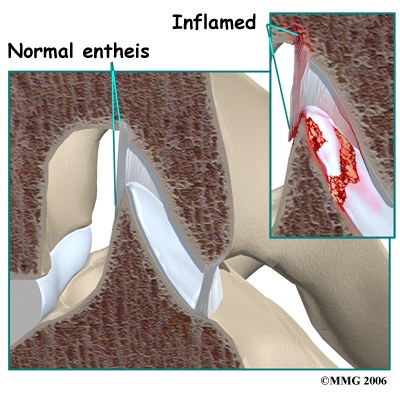
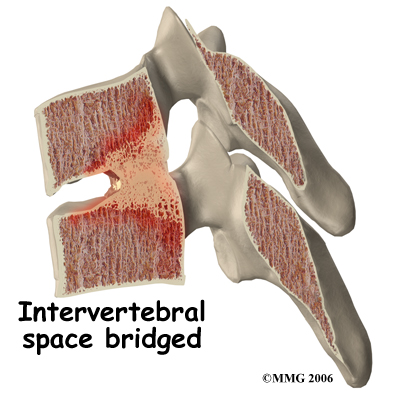
 In some rheumatological diseases, the inflammatory process affects other areas of connective tissue such as where ligaments and tendons attach to the bone. This area is called an enthesis. There are entheses located all over the body with many in the spine itself, such as where the intervertebral disc attaches to the vertebra. Many of the rheumatological diseases that affect the spine seem to attack these particular areas of the spine but it is unclear why this occurs.
In some rheumatological diseases, the inflammatory process affects other areas of connective tissue such as where ligaments and tendons attach to the bone. This area is called an enthesis. There are entheses located all over the body with many in the spine itself, such as where the intervertebral disc attaches to the vertebra. Many of the rheumatological diseases that affect the spine seem to attack these particular areas of the spine but it is unclear why this occurs.
Related Document: Combined Therapy Specialties Guide to Lumbar Spine Anatomy
Causes
What causes this problem?
The cause, or causes, of rheumatological disease is still unknown. There is increasing evidence that the underlying cause in many of these conditions is a combination of a person's genetic makeup and how that individual responds to certain types of infections.
For many years, doctors have been aware that people with these diseases have a higher percentage of a gene called HLA-B27. The HLA-B27 gene plays a role in determining how the cells of the body react against infection. Not everyone with this gene will develop a rheumatological disease, but the vast majority of people with any of the rheumatological diseases have the gene. Recently, more research has shown that there are a number of variations of the HLA-B27 gene. This further complicates attempts understand what role genetics plays in the cause of these diseases.
There are also a number of different infections that have been found to be related to the development of rheumatological diseases. When patients with these diseases are studied, there seems to be certain bacterial infections that are more likely to precede the development of the rheumatological disease. The infection may be over, but the body continues to mount an inflammatory response that goes on to attack the connective tissue structures of the body itself.
The current evidence suggests that people with certain genes are more likely to react to specific types of infections by developing a rheumatological disease.
Symptoms
What does the condition feel like?
Pain and stiffness are the primary symptoms reported in the spine in patients with a rheumatological disease. The pain and stiffness is worse in the morning and improves with activity. The flexibility of the spine decreases as time passes and the disease progresses.
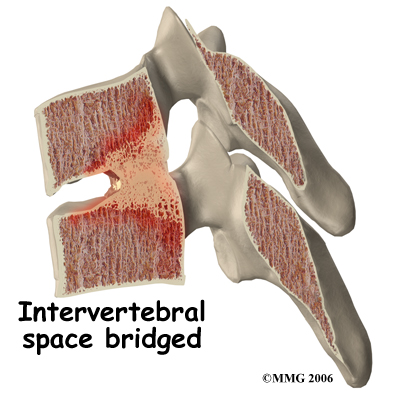
In diseases that affect the synovial joints, destruction of the joints can result in instability of the spine and may cause pressure on the spinal nerves or spinal cord. In the diseases that affect the entheses, the spine more commonly develops large bone spurs and may fuse together and become stiff. Instability also occurs if the stiff spine is fractured.
These diseases are systemic, meaning that they affect the entire body, so symptoms are also felt in other areas outside of the spine such as the other synovial joints, and the other entheses of the body. The sacroiliac joints, hips, knuckles, and shoulders are common areas of pain. The exact location of symptoms depends on the type of spondyloarthropathy present. Some of the diseases may include a skin rash, such as psoriasis. Several of the spondyloarthropathies affect the eyes, causing uveitis (inflammation of the iris).
Inflammation of the urethra (the tube from the bladder to the outside) can occur and causes pain when urinating, called urethritis. Ankylosing Spondylitis (AS) can also affect the gut, aorta, or heart. All of the symptoms mentioned here are called extraskeletal manifestations. This means the symptoms affect some part of the body other than the tendons and bones.
Related Document: Combined Therapy Specialties Guide to Rheumatoid Arthritis
Diagnosis
How do health care professionals diagnose the problem?
The diagnosis requires a careful history followed by a thorough physical examination. Many patients have someone directly related to them that suffers from the same disease. Your doctor may ask questions about symptoms of recent infections such as diarrhea, burning with urination, difficulty with vision, or eye pain.
The laboratory evaluation is very useful in the diagnosis. Tests such as C-reactive protein (CRP) level and erythrocyte sedimentation rate (ESR) may be ordered to look for signs of infection and chronic inflammation. Other tests can be done for rheumatoid arthritis and the presence of the HLA-B27 gene. The HLA-B27 gene, however, is not always present in patients with a spondyloarthropathy and it may also be present in normal, healthy individuals without a spondyloarthropathy, so unfortunately it can not be used to definitively diagnose the presence of the disease.
Analysis of synovial fluid may be needed to rule out septic (infectious) arthritis of the joints. Additional tests may be ordered for patients with inflammatory bowel disease (IBD) or when reactive arthritis is suspected.
X-rays can be very useful to show the changes in the spine, joints and pelvis that are common with many of these diseases. X-rays are usually the first test ordered before any of the more specialized tests. In the early stages the x-rays may be negative, but as time passes, the changes may appear and confirm the diagnosis.

Other radiological imaging tests may also be useful. A bone scan can show the sites of inflammation before the changes appear on x-rays. A bone scan is a special test where radioactive tracers are injected into your blood stream. The tracers then show up on special x-rays of your back. The tracers build up in areas where bone is undergoing a rapid repair process, such as a healing fracture or the area surrounding an infection or tumor. Usually the bone scan is used to locate the problem. Other tests such as the computed tomography (CT) scan or magnetic resonance imaging (MRI) scan are then used to look at the area in detail.
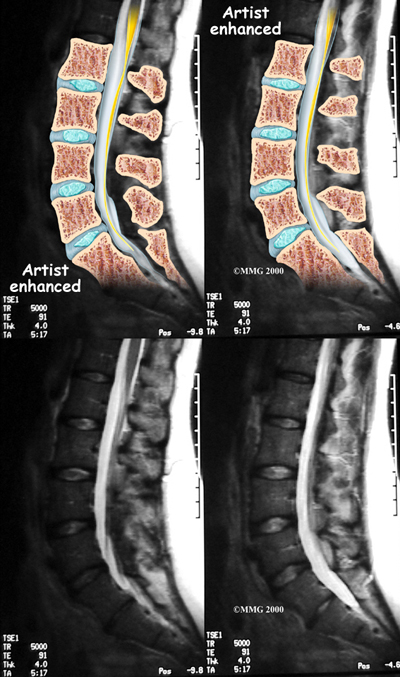
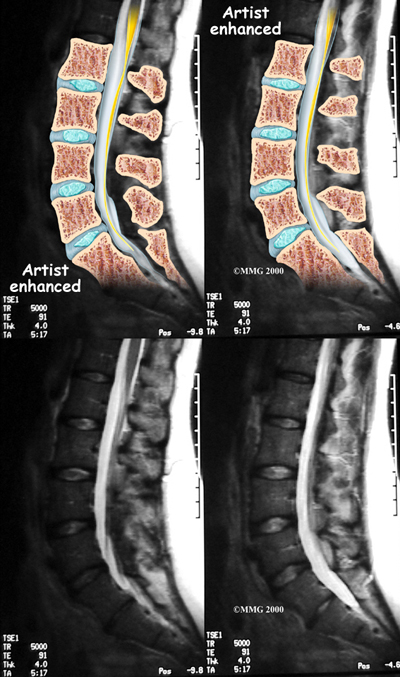
If there are symptoms suggesting the spinal nerves or spinal cord are in danger, an MRI scan may be recommended to look at the spine more closely. The MRI scan uses magnetic waves to create pictures of the lumbar spine in slices. The MRI scan shows the lumbar spine bones as well as the soft tissue structures such as the discs, joints and nerves. MRI scans are painless and don't require needles or dye. Specialized MRI techniques are now available that can detect inflammatory changes in the sacroiliac and vertebral joints long before they appear on x-rays.
Treatment
What treatment options are available?
Currently there is no cure for spondyloarthropathies. The goal of treatment is to manage the pain and, when possible, to slow the progression of the damage to the underlying structures.
If you smoke or use tobacco products, long-term outcomes are worse. You should quit as soon as possible. A health care professional can help you with this important step.
Medications and physical therapy are the primary tools available for treatment.
Medications
 Non-steroidal anti-inflammatory drugs (NSAIDs) are the main drugs used for treatment of the pain associated with these diseases. These drugs include aspirin, ibuprofen, indomethacin and naprosyn. There are others in the group as well. These drugs reduce the inflammation and control pain. There is no evidence that they stop or slow the progression of the disease.
Non-steroidal anti-inflammatory drugs (NSAIDs) are the main drugs used for treatment of the pain associated with these diseases. These drugs include aspirin, ibuprofen, indomethacin and naprosyn. There are others in the group as well. These drugs reduce the inflammation and control pain. There is no evidence that they stop or slow the progression of the disease.
Cortisone can be used to control flare-ups of pain. Cortisone is a powerful anti-inflammatory medication. When used for short periods of time, the medication is safe and well tolerated. When used continuously over a period of months, the side effects can be significant. Your doctor will not want to use cortisone for a prolonged period if at all possible. In some cases, however, such as with advanced rheumatoid arthritis, it may become necessary to use cortisone indefinitely to control the disease.
There are newer medications that have been developed to control rheumatoid arthritis that are sometimes beneficial in the spondyloarthropathies. Some of these medications actually slow the progression of the damage from the disease. These medications are known as disease modifying anti-rheumatic drugs (DMARDs). DMARDs include gold injections, methotrexate, sulfasalazine and azothioprine. These medications may be used primarily to control the symptoms in other parts of the body, but may also improve the spinal disease as well.
Recently, new medications have been available that may prove to be very beneficial for these diseases. One of the chemicals in the body that seems to make the inflammation worse in these diseases is tumor necrosis factor (TNF). Drugs that block the effect of this chemical are called tumor necrosis factor-a inhibitors. TNF-a inhibitors are have recently begun to be used to treat a variety of inflammatory diseases. These drugs have shown promise in helping to control the inflammation and symptoms of the spondyloarthropathies as well. TNF-a inhibitors result in dramatic decreases in CRP levels and ESR improvements are also seen on MRIs.
Treatment with TNF-a inhibitors must be kept up over the long-term to stay in control of the disease. If one agent doesn't work, your doctor may switch you to another. There are some serious side effects with these agents, so they aren't used with everyone. We don't know yet if these agents will prevent the bony changes that lead to spinal fusion. More research is needed to determine this.
Surgery is rarely indicated in the treatment of these diseases, except where the damage caused by the disease has caused pressure on the spinal nerves or spinal cord. Total joint replacements may be needed for patients with severe damage to the hip or knee. Some patients elect to have surgery to correct kyphosis (forward curve or humpback of the upper spine) or to correct spine instability that has occurred from a fracture.
Physical therapy
Remaining as active as possible is critical to maintaining your function when you have a spondyloarthropathy. At Combined Therapy Specialties we can advise you on how best to stay active and teach you how to maximize your function and retain as much flexibility as possible.
On your first visit to Combined Therapy Specialties your physical therapist will take a detailed history from you and will ask you information about the symptoms in your spine, as well the symptoms you may experience in any other areas of your body. We will also discuss your goals with regards to physical therapy treatment. It is important for us to know how physically active you have been in the past and if you have been able to keep up your activity since you have developed symptoms. Your physical therapist will also want to know if your symptoms follow a pattern, such as being worse in the morning or after periods of inactivity, or if they get better or worse with certain physical activities or during particular seasons or times of the month. Any details you can provide regarding treatments that you have found that decrease your symptoms will also be useful for us when we are developing a plan to maximize your function. It will also be important for us to know which medications you have been taking to manage your symptoms, and how effective you feel these medications are so we can also factor this into our treatment plan for you. If you feel your medications have not been that useful, we will ask you to follow-up with your doctor immediately to discuss this.
At Combined Therapy Specialties we believe that in order to help manage your symptoms, you should learn as much as you can about your disease and what you can do to control your symptoms and remain as healthy as possible. For this reason, we will educate you about the spondyloarthropathy process but we will also encourage you to do some research for yourself. Support groups are available online and in many cities where people can come together and help with information and support and can be extremely valuable in managing a chronic disease. Getting advice and guidance from someone who has experience with the disease and can provide tips and pointers for living with the disease on a daily basis can be extremely valuable.
During times where your symptoms flare-up, a series of physical therapy sessions at Combined Therapy Specialties will be useful. During these sessions, your therapist can do several things to ease your symptoms, such as use massage, manual therapy, electrical modalities, as well as ice or heat. If you are willing, some of our physical therapists may even choose to use acupuncture or a form of dry needling to ease your symptoms. Our therapy, however, will be most useful in managing your acute flare-ups. For longer-term management, we will encourage you to be physically active, partake in some aerobic activity, and will provide you will a specific home exercise program of stretches and strengthening exercises designed to maintain the mobility and strength in both your spine and any other joints that have been affected.
Specifically regarding your spine, maintaining extension and rotation of your entire spine is particularly important, as it is these motions which are most often lost due to the chronic inflammation that occurs with a spondyloarthropathy. Your physical therapist will show you flexibility exercises to maintain the mobility of your entire spine, and will ask you to do these as part of a regular home program.
Your physical therapist will also stress the importance of using proper upright posturing as often as possible to maintain the mobility in your spine, and decrease the stress on your other joints. An upright posture will also help to maintain your spine in the most optimal alignment so that if some fusion does occur, your spine is in the most functional position possible.
Maintaining erect spinal posture and flexibility also requires the muscles of your spine to remain strong. Your physical therapist will focus on teaching you how to activate your core muscles supporting the spine, which increase your stability and work to keep the spine in the upright posture. Strengthening exercise for your back and neck muscles will also be added to your home exercise program to ensure you maintain the strength to oppose the common forward flexed position of the spine.
If your upper spine does start to curve forward as a result of the spondyloarthropathy, you will also lose the ability to reach your arms into their full range of motion overhead. Losing this ability can be very limiting when trying to perform activities of daily living such as combing the back of your hair, or reaching to the top of the refrigerator, and it is extremely limiting if you partake in any overhead sporting activities. For this reason your physical therapist will also show you home exercises that help maintain your shoulder range of motion particularly up into the overhead position.
A flexed and stiff spine will also affect your capacity to breathe deeply because the space for your lungs is decreased. Deep breathing exercises will be an important part of your home program. These exercises will help to maintain your lung volume as well as help the joints of your ribs and thoracic spine move through their range of motion and maintain their mobility. During aerobic exercise you will naturally take these deep breaths, which is another reason your physical therapist will encourage you to partake in some aerobic exercise as part of your home program.
Participating in aerobic activity and remaining physically active can be the key to long-term management of spondyloarthropathy symptoms. Your physical therapist will discuss with you the best aerobic activities to partake in, but as a general rule, low-impact activities such as walking, swimming, or cycling are better for your joints over the long-term. If you have not previously done much aerobic exercise your physical therapist will discuss an appropriate exercise mode for you to begin. He or she can design your activity program to start out slowly and build up to a moderate amount of exercise which you can maintain. It will be best if you can partake in some form of aerobic activity on most days of the week as well as incorporate your home exercises for flexibility into the majority of the days as well. Being physically active also means doing things such as taking the stairs instead of the elevator, or walking rather than driving if you are able to. Due to the symptoms of spondyloarthropathies flaring up at times, and being less symptomatic at times, it is recommended that to protect your joints, you partake in aerobic exercise when you are not experiencing a flare-up. Some patients will find, however, that low-impact aerobic activity can actually help to ease a flare-up. In these cases, it is obviously recommended to continue your exercise during this time as able.
By following your physical therapist’s advice on exercise, coming for treatment during times when the symptoms flare-up, as well as seeing your doctor for regular check-ups and medication reviews, most people are able to effectively manage their symptoms of a spondyloarthropathy and live a normal active life.
Portions of this document copyright MMG, LLC.
Combined Therapy Specialties provides services for physical therapy in Asheville.








 In some rheumatological diseases, the inflammatory process affects other areas of connective tissue such as where ligaments and tendons attach to the bone. This area is called an enthesis. There are entheses located all over the body with many in the spine itself, such as where the intervertebral disc attaches to the vertebra. Many of the rheumatological diseases that affect the spine seem to attack these particular areas of the spine but it is unclear why this occurs.
In some rheumatological diseases, the inflammatory process affects other areas of connective tissue such as where ligaments and tendons attach to the bone. This area is called an enthesis. There are entheses located all over the body with many in the spine itself, such as where the intervertebral disc attaches to the vertebra. Many of the rheumatological diseases that affect the spine seem to attack these particular areas of the spine but it is unclear why this occurs.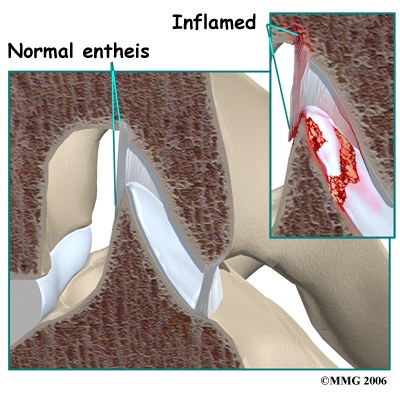

 Non-steroidal anti-inflammatory drugs (NSAIDs) are the main drugs used for treatment of the pain associated with these diseases. These drugs include aspirin, ibuprofen, indomethacin and naprosyn. There are others in the group as well. These drugs reduce the inflammation and control pain. There is no evidence that they stop or slow the progression of the disease.
Non-steroidal anti-inflammatory drugs (NSAIDs) are the main drugs used for treatment of the pain associated with these diseases. These drugs include aspirin, ibuprofen, indomethacin and naprosyn. There are others in the group as well. These drugs reduce the inflammation and control pain. There is no evidence that they stop or slow the progression of the disease.
