Introduction
Physical therapy in Asheville for Lower Back
Welcome to Combined Therapy Specialties patient guide on spinal compression fractures.
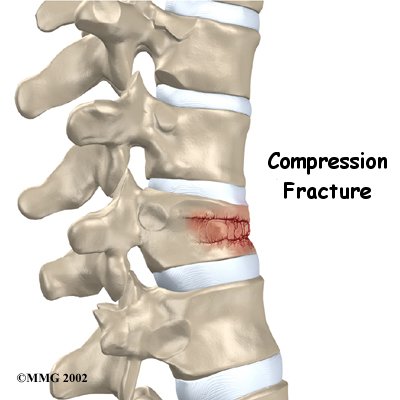
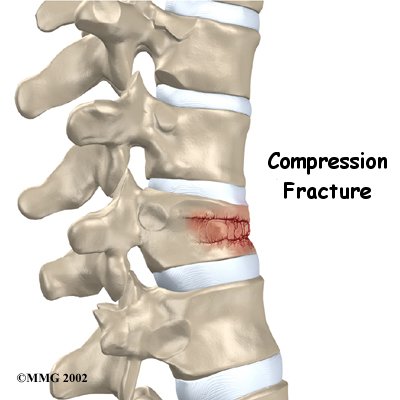
Compression fractures are the most common type of fracture affecting the spine. A compression fracture of a spine bone (vertebra) causes the bone to collapse in height.
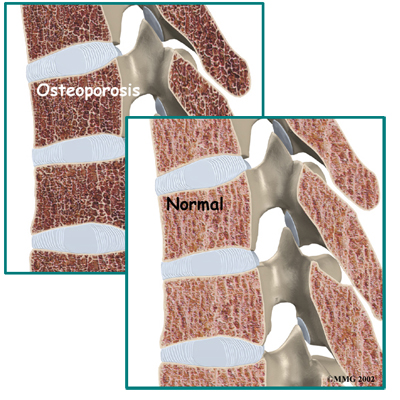
Compression fractures are commonly the result of osteoporosis. About 700,000 cases of compression fractures due to osteoporosis occur each year in the United States. Spinal bones that are weakened from osteoporosis may become unable to support normal stress and pressure. As a result, something as simple as coughing, twisting, or lifting can cause a vertebra to fracture.
An injury to the spine, such as from a hard fall on the buttocks or blow to the head, can cause a spinal compression fracture. Compression fractures may also occur if cancer from other parts of the body spreads to the spine. Cancer weakens the spinal bones and makes them prone to fractures.
This guide will help you understand:
- how compression fractures happen
- how your health care professional will diagnose the condition
- what treatment options are available
- what Combined Therapy Specialties approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
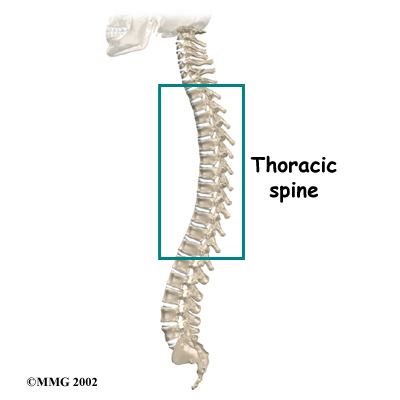
The human spine is made of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to create the spinal column. The spinal column gives the body its form. It is the body's main upright support.
The main section of each vertebra is a large, round structure called a vertebral body.
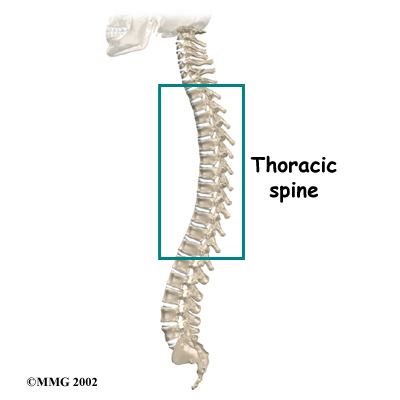
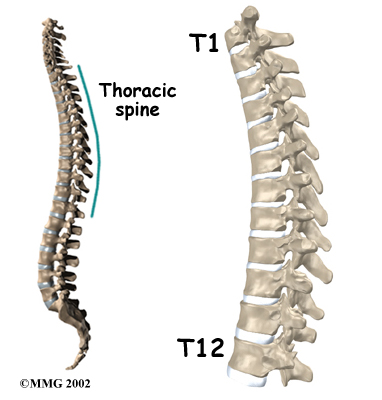
Compression fractures cause this section of bone to collapse. When the fracture is due to osteoporosis, it usually occurs in the lower part of the thoracic spine, near the bottom of the rib cage.
A bony ring attaches to the back of each vertebral body. When the vertebrae are stacked on one another, the bony rings form a hollow tube. This tube, or canal, surrounds the spinal cord. The spinal cord is like a long wire made of millions of nerve fibers. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.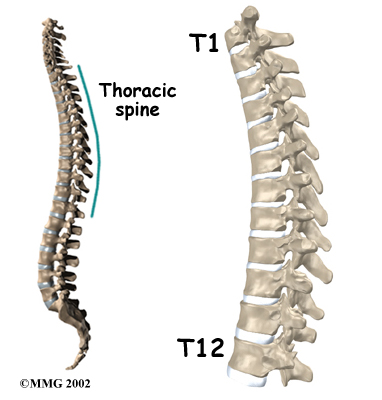
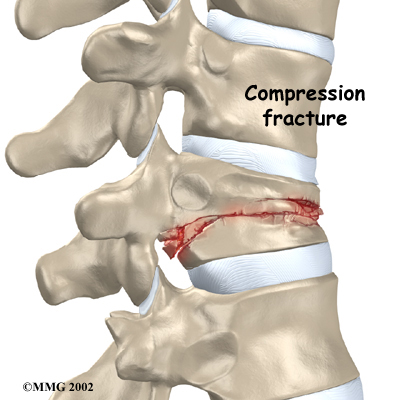
Severe from forceful impact on the spine, as can happen in a car accident, can cause fragments of the vertebral body to push into the spinal canal and press against the spinal cord. This can cause damage to the spinal cord that can result in partial or complete paralysis below the waist. It is rare for a typical compression fracture from osteoporosis to cause damage to the spinal cord.
Causes
Why do I have this problem?
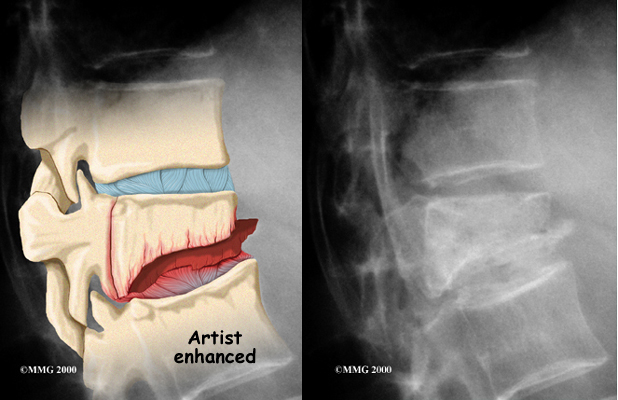
 Strong, healthy bones are able to withstand the forces and strains of normal activity. Compression fractures in the spine happen when either the forces are too great or the bones of the spine aren't strong enough. The vertebral body cracks under pressure. Fractures from forceful impact on the spine tend to crack the back (posterior) part of the vertebral body. Fractures from osteoporosis usually occur in the front (anterior) part of the vertebral body.
Strong, healthy bones are able to withstand the forces and strains of normal activity. Compression fractures in the spine happen when either the forces are too great or the bones of the spine aren't strong enough. The vertebral body cracks under pressure. Fractures from forceful impact on the spine tend to crack the back (posterior) part of the vertebral body. Fractures from osteoporosis usually occur in the front (anterior) part of the vertebral body.
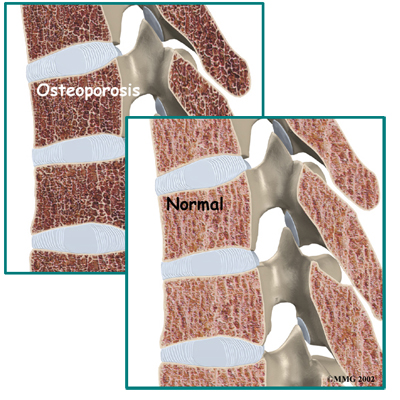
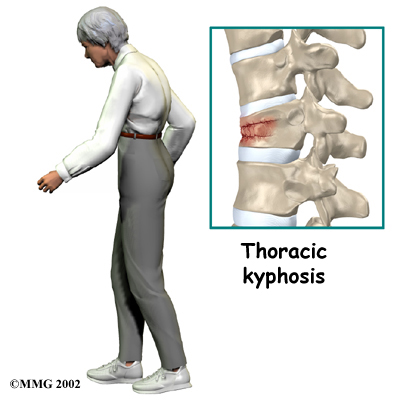
is a disease that weakens bone. Sometimes the bones in the spine weaken to the point that even mild forces can lead to a compression fracture. A simple action like reaching down to pull on a pair of socks can cause a weakened vertebra to fracture. The front of the vertebra (the part closest to the front of the body) crumbles, causing the round vertebral body to become wedge-shaped. This angles the spine forward, producing a hunch-backed appearance, called kyphosis.
Diseases or conditions that affect the parathyroid gland can also weaken bones. Four pea-sized parathyroid glands are located just behind the thyroid gland in the throat. They produce a substance called parathyroid hormone (PTH), which normally regulates the amount of calcium in the blood stream. An overactive parathyroid gland releases too much PTH, causing the body to leach calcium from bones, even when there is more than enough calcium circulating in the blood stream. This disorder is called hyperparathyroidism. It occurs when a tumor, called an adenoma, forms in one of the parathyroid glands. Cancers that affect the kidney, skin, or parathyroid gland may also cause the parathyroid gland to malfunction. If the problem isn't fixed, bones continue to lose calcium and eventually weaken. Weakening in the spine bones makes the vertebrae more prone to crack in front, as is typical with osteoporosis.
Cancers that form in other parts of the body have a tendency to spread, or metastasize, to the spine. When this happens, the cancer weakens the spinal bones, making them susceptible to compression fractures. Doctors may suspect unrecognized cancer if a patient has a compression fracture without any particular cause or reason.
Spine trauma can produce mild or severe compression fractures. Compression fractures from trauma usually involve high forces that impact the spine when it is bent forward. This is typically what happens when a person falls onto the buttocks or strikes his head on the windshield in a car accident. Again, these traumatic fractures usually affect the back part of the vertebral body.
Combined Therapy Specialties Guide to Osteoporosis
Symptoms
What does the condition feel like?
Compression fractures caused by thin, weakened bones may cause little or no pain at first. Sometimes pain is centered over the area where the fracture has occurred. The collapsed vertebra gives the spine a hunched appearance, and the loss of vertebral height shortens the muscles on each side of the spine. This forces the back muscles to work harder, causing muscle fatigue and pain. When pain does occur, it usually goes away after a few weeks. However, back pain sometimes escalates to the point that patients seek medical help.
Traumatic compression fractures can produce intense pain in the back that spreads into the legs. If the fracture severely damages the vertebral body, bone fragments may lodge in the spinal canal, pressing on the spinal cord. This can paralyze muscles and impair sensation in the areas supplied by the damaged nerve tissue. Such a fracture may also cause the spine to become unstable. When this happens, the spine eventually tilts forward into increased kyphosis, and the potential grows for future complications with the spinal cord.
Diagnosis
How do health care professionals diagnose the problem?
Diagnosis begins with a complete history and physical examination. Your physical therapist at Combined Therapy Specialties will ask questions about your symptoms and how your problem is affecting your daily activities. These include questions about where you feel pain, when the pain started, what you were doing when the pain started, and if you have numbness or weakness in your limbs. Your physical therapist will also want to know what positions or activities make your symptoms worse or better.
Next your physical therapist will do a physical examination. They will palpate, or touch, gently along your spine and surrounding tissues to determine the exact location of pain. Compression fractures often cause soreness and tenderness in the area over or near the fractured vertebra. Next they will ask you to actively move in different directions to determine which back movements cause pain or other symptoms and assess how restricted your range of motion is. Your skin sensation, muscle strength, and reflexes may also require testing. In addition, your physical therapist may also examine your hip joints as they are closely related to the proper functioning of the back.
If your physical therapist deducts from the history and physical examination that your problem is potentially due to a compression fracture, we will refer you on to your doctor for further examination and investigations to help confirm this suspicion.
Combined Therapy Specialties Guide to Osteoporosis
Physician’s Review
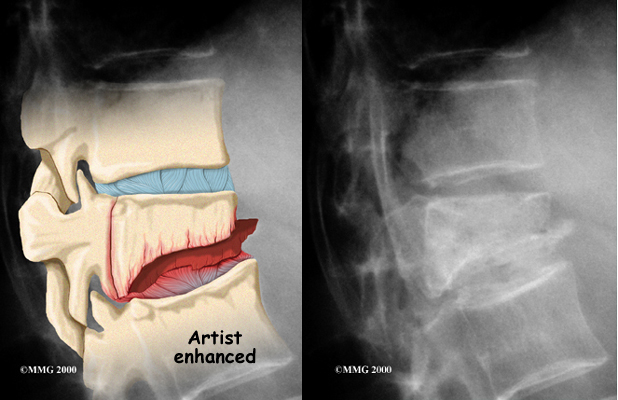 If your doctor believes there is a compression fracture, are ordered. X-rays can show fractures of the vertebrae.
If your doctor believes there is a compression fracture, are ordered. X-rays can show fractures of the vertebrae.
When an X-ray confirms a compression fracture, computed tomography (a CT scan) may be ordered. This is a detailed X-ray that lets the doctor see slices of the body's tissue. The image can show whether the compression fracture has caused the area to become unstable from the injury.
If symptoms suggest problems with the spinal cord, the doctor may combine the CT scan with myelography. To do this, a special dye is injected into the space around the spinal canal (the subarachnoid space). When the CT scan is performed, the dye highlights the spinal cord and spinal nerves. The dye can improve the accuracy of a standard CT scan for diagnosing the health of the spinal cord and spinal nerves.
Magnetic resonance imaging (MRI) can show the doctor problems affecting the nerves or causing pain. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. It shows problems in other soft tissues such as the discs and spinal cord. This machine creates pictures that look like slices of the area your doctor is interested in. The test does not require special dye or a needle.
Your doctor may order a bone scan to get additional information. This involves injecting chemical tracers into your blood stream. The tracers then show up on special X-rays of your spine. The tracers build up in areas of extra stress to bone tissue. This test can show if there are any old compression fractures, which would alert the doctor to problems with osteoporosis. If you have osteoporosis, the doctor will suggest ways to prevent future problems.
Treatment
What treatment options are available?
Nonsurgical Treatment
 The majority of patients with compression fractures are treated without surgery. Most compression fractures heal within eight weeks with simple remedies of medicine, rest, rehabilitation, and a special back brace.
The majority of patients with compression fractures are treated without surgery. Most compression fractures heal within eight weeks with simple remedies of medicine, rest, rehabilitation, and a special back brace.
Most patients are given medication to control pain. Although medications can help ease pain, they are not designed to heal the fracture. With pain under control, patients find it easier to get up and move about, avoiding the problems that come from remaining immobile in bed.
Patients are usually prescribed a short period of rest. This gives the fracture a chance to heal and aids in pain control. In some extreme cases, the doctor may have a patient stay in bed for up to one week.
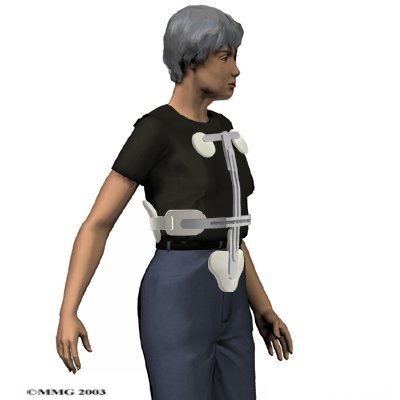
Most patients are fit with a special back brace, called an orthosis. This type of brace is molded to the patient's body. It limits spine movement in general, though the brace is usually fashioned to keep patients from bending forward. This protects the fractured vertebral body so it can heal and also assists with pain relief. Patients who wear a special brace will be advised to move about as normal but to limit strenuous activities, such as lifting and bending.
Rehabilitation
What should I expect as I recover?
Most spinal compression fractures caused by osteoporosis get better within approximately eight weeks. As mentioned, most patients who suffer compression fractures from osteoporosis don't require surgery. Instead they are treated conservatively with rest, bracing and a few rehabilitation sessions early on for pain relief and education regarding self-management.
Rehabilitation after traumatic vertebral fractures, unfortunately, can be a much slower process. In these cases, patients sometimes need to attend therapy for two to three months and should expect full recovery to take up to one year.
Physical therapy treatment for a spinal compression fracture at Combined Therapy Specialties usually begins once the fracture has been positively confirmed on investigation and has been determined to be stable. If a period of relative bed rest has been prescribed, physical therapy will begin after this rest has been adhered to.
Your initial treatment at Combined Therapy Specialties will aim to decrease the inflammation and pain caused near the area of the compression fracture. Your physical therapist may use electrical modalities such as ultrasound or interferential current to ease these symptoms. Massage to the muscles or other hands-on techniques such as gentle traction to the joints may also be helpful. Often applying ice or heat to the painful area can also drastically ease the symptoms.
Fortunately, with the assistance of rehabilitation, the back pain caused directly from the fracture generally improves as the fracture heals. However, the fracture changes the way the spine works, so it is not unusual for patients to have some lingering soreness in the muscles and joints near the fractured vertebra. If there is a significant amount of pain that remains ongoing your physical therapist will recommend that you return to your doctor for further discussions on managing the pain through medications.
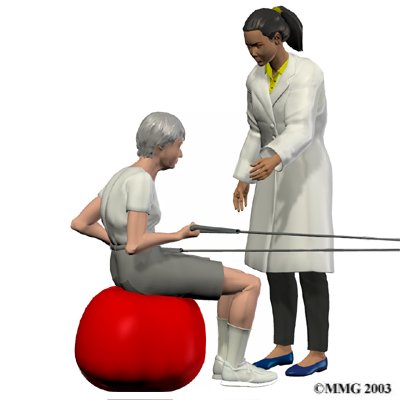
As the pain from the compression fracture begins to subside, your physical therapist at Combined Therapy Specialties will begin to focus on improving any flexibility and strength deficits you may have developed from the period of decreased activity following the compression fracture.
 Your physical therapist will prescribe exercises for you to do in the clinic and also to be done as part of a home program. Exercises that improve the range of motion in your back, neck, shoulders as well as your hips may be prescribed. If your compression fracture was from osteoporosis, then the extension motion of your upper back (thoracic spine) will be of paramount importance. As mentioned above, wedge compression fractures of the thoracic spine from osteoporosis often lead to a flexed back posture. The risk of losing the ability to function in the upright extended position is high so maintaining this motion is crucial. Even the proper use of your shoulder joints will suffer if the spine loses extension therefore exercises may also be prescribed to maintain shoulder function. Neck range of motion can also be affected if the flexed posturing becomes severe thus range of motion exercises for the neck may also be required. Hip range of motion deficits will be addressed as normal hip range of motion allows the spine to move more freely and decreases the stress on the spinal joints. Patients with traumatic stress fractures don’t often present with the wedge shaped fractures and therefore the primary focus will be the recovery of all ranges of motion, not just thoracic extension.
Your physical therapist will prescribe exercises for you to do in the clinic and also to be done as part of a home program. Exercises that improve the range of motion in your back, neck, shoulders as well as your hips may be prescribed. If your compression fracture was from osteoporosis, then the extension motion of your upper back (thoracic spine) will be of paramount importance. As mentioned above, wedge compression fractures of the thoracic spine from osteoporosis often lead to a flexed back posture. The risk of losing the ability to function in the upright extended position is high so maintaining this motion is crucial. Even the proper use of your shoulder joints will suffer if the spine loses extension therefore exercises may also be prescribed to maintain shoulder function. Neck range of motion can also be affected if the flexed posturing becomes severe thus range of motion exercises for the neck may also be required. Hip range of motion deficits will be addressed as normal hip range of motion allows the spine to move more freely and decreases the stress on the spinal joints. Patients with traumatic stress fractures don’t often present with the wedge shaped fractures and therefore the primary focus will be the recovery of all ranges of motion, not just thoracic extension.
In addition to range of motion exercises, your Combined Therapy Specialties physical therapist will also prescribe strengthening exercises which focus on the deep abdominal muscles for overall support of the spine, as well as exercises to strengthen the back muscles which resist the forward bending of the spine. For patients with osteoporosis, it is important to include weight bearing exercise such as walking or stair climbing. Bone reacts to increase stress by producing more bone, which increases its overall strength. The added stress of simple weight bearing activities therefore works to encourage stronger bones. Your physical therapist may also prescribe exercises for you using light weights for the same reason of encouraging the build up of overall bone strength.
At Combined Therapy Specialties we believe that education for our patients is of utmost importance therefore discussions on how to improve and maintain your posture will be a large focus of our treatment. Your physical therapist will discuss proper body mechanics when moving in order to keep your back in safe positions and avoid extra strain near the fracture as you go about your work and daily activities. We will discuss positions you use when sitting, lying down, standing, and walking as well as safe body mechanics with lifting, carrying, pushing, and pulling. We will also educate patients with osteoporosis on the proper techniques for simple daily activities such as coughing or sneezing, which due to the forceful flexion involved, can result in another compression fracture in those with particularly frail bones. Falling can also easily result in fractures of osteoporotic bones so balance activities may be added to your home program to decrease the likelihood of a fall occurring. The goal of rehabilitation at Combined Therapy Specialties is for you is to improve your posture, body mechanics, strength, and flexibility so as to avoid future injuries.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Surgery
Open surgical treatment for spinal compression fractures due to osteoporosis is rarely needed. (Open procedures require larger incisions to give the surgeon more room to operate.) In rare cases of severe trauma, however, open surgery is sometimes required. Open surgery is done if the spinal segment has loosened and bone fragments have damaged the spinal cord and spinal nerves.
Surgeons have begun using two new procedures to treat compression fractures caused by osteoporosis. Both are considered minimally invasive. Minimally invasive means the incisions used are very small, and there is little disturbance of the muscles and bones where the procedure is done. These two procedures help the fracture heal and avoid the problems associated with more involved surgeries.
These new procedures are:
- vertebroplasty
- kyphoplasty
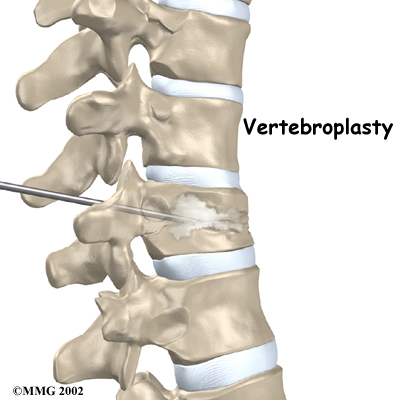
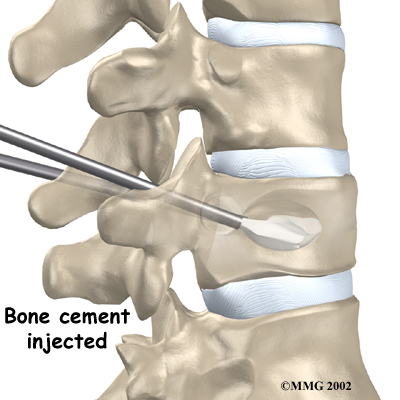
Vertebroplasty
This procedure is most helpful for reducing pain. It also strengthens the fractured bone, enabling patients to rehabilitate faster.
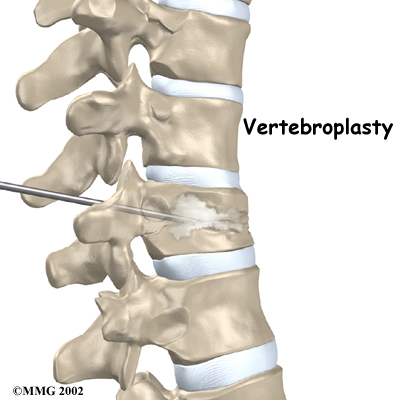
To perform vertebroplasty, the surgeon uses a fluoroscope to guide a needle into the fractured vertebral body. A fluoroscope is a special X-ray television that allows the surgeon to see your spine and the needle as it moves. Once the surgeon is sure the needle is in the right place, bone cement, called polymethylmethacrylate (PMMA), is injected through the needle into the fractured vertebra. A reaction in the cement causes it to harden within 15 minutes. This fixes the bone so that it does not collapse any further as it heals. More than 80 percent of patients get immediate pain relief with this procedure.
Combined Therapy Specialties Guide to Vertebroplasty
Kyphoplasty
Kyphoplasty is another way for surgeons to treat vertebral compression fractures. Like vertebroplasty, this procedure halts severe pain and strengthens the fractured bone. However, it also gives the advantage of improving some or all of the lost height in the vertebral body, helping prevent kyphosis.
Two long needles are inserted through the sides of the spinal column into the fractured vertebral body. These needles guide the surgeon while drilling two holes into the vertebral body. The surgeon uses a fluoroscope (mentioned above) to make sure the needles and drill holes are placed in the right spot.
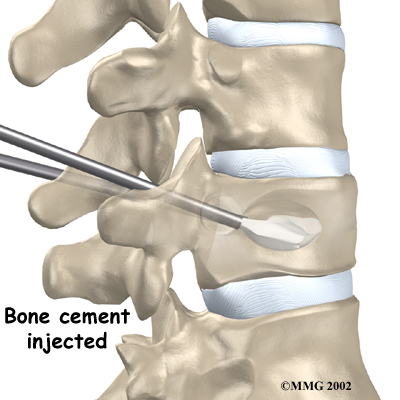
The surgeon then slides a hollow tube with a deflated balloon on the end through each drill hole. Inflating the balloons restores the height of the vertebral body and corrects the kyphosis deformity. Before the procedure is complete, the surgeon injects bone cement into the hollow space formed by the balloon. This fixes the bone in its corrected size and position.
A Patient's Guide to Kyphoplasty
Portions of this document copyright MMG, LLC.







 Strong, healthy bones are able to withstand the forces and strains of normal activity. Compression fractures in the spine happen when either the forces are too great or the bones of the spine aren't strong enough. The vertebral body cracks under pressure. Fractures from forceful impact on the spine tend to crack the back (posterior) part of the vertebral body. Fractures from osteoporosis usually occur in the front (anterior) part of the vertebral body.
Strong, healthy bones are able to withstand the forces and strains of normal activity. Compression fractures in the spine happen when either the forces are too great or the bones of the spine aren't strong enough. The vertebral body cracks under pressure. Fractures from forceful impact on the spine tend to crack the back (posterior) part of the vertebral body. Fractures from osteoporosis usually occur in the front (anterior) part of the vertebral body.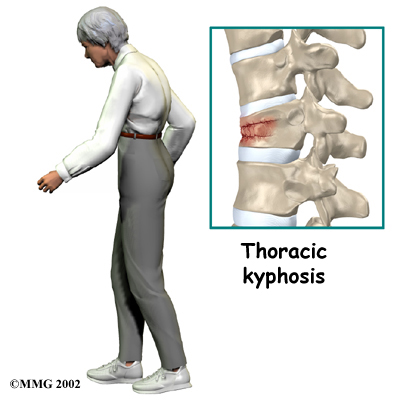
 If your doctor believes there is a compression fracture,
If your doctor believes there is a compression fracture, 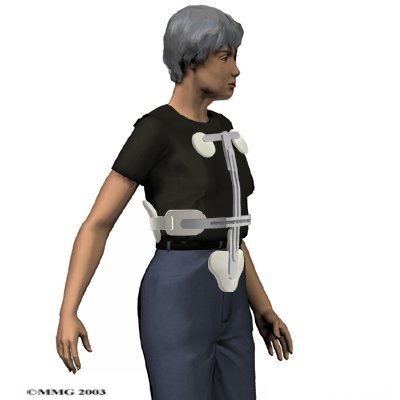 The majority of patients with compression fractures are treated without surgery. Most compression fractures heal within eight weeks with simple remedies of medicine, rest, rehabilitation, and a special back brace.
The majority of patients with compression fractures are treated without surgery. Most compression fractures heal within eight weeks with simple remedies of medicine, rest, rehabilitation, and a special back brace.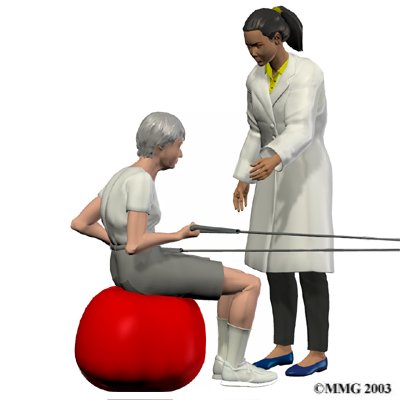 Your physical therapist will prescribe exercises for you to do in the clinic and also to be done as part of a home program. Exercises that improve the range of motion in your back, neck, shoulders as well as your hips may be prescribed. If your compression fracture was from osteoporosis, then the extension motion of your upper back (thoracic spine) will be of paramount importance. As mentioned above, wedge compression fractures of the thoracic spine from osteoporosis often lead to a flexed back posture. The risk of losing the ability to function in the upright extended position is high so maintaining this motion is crucial. Even the proper use of your shoulder joints will suffer if the spine loses extension therefore exercises may also be prescribed to maintain shoulder function. Neck range of motion can also be affected if the flexed posturing becomes severe thus range of motion exercises for the neck may also be required. Hip range of motion deficits will be addressed as normal hip range of motion allows the spine to move more freely and decreases the stress on the spinal joints. Patients with traumatic stress fractures don’t often present with the wedge shaped fractures and therefore the primary focus will be the recovery of all ranges of motion, not just thoracic extension.
Your physical therapist will prescribe exercises for you to do in the clinic and also to be done as part of a home program. Exercises that improve the range of motion in your back, neck, shoulders as well as your hips may be prescribed. If your compression fracture was from osteoporosis, then the extension motion of your upper back (thoracic spine) will be of paramount importance. As mentioned above, wedge compression fractures of the thoracic spine from osteoporosis often lead to a flexed back posture. The risk of losing the ability to function in the upright extended position is high so maintaining this motion is crucial. Even the proper use of your shoulder joints will suffer if the spine loses extension therefore exercises may also be prescribed to maintain shoulder function. Neck range of motion can also be affected if the flexed posturing becomes severe thus range of motion exercises for the neck may also be required. Hip range of motion deficits will be addressed as normal hip range of motion allows the spine to move more freely and decreases the stress on the spinal joints. Patients with traumatic stress fractures don’t often present with the wedge shaped fractures and therefore the primary focus will be the recovery of all ranges of motion, not just thoracic extension.