Introduction
Physical therapy in Asheville for Hip Issues
Welcome to Combined Therapy Specialties Guide to Avascular Necrosis of the Hip.
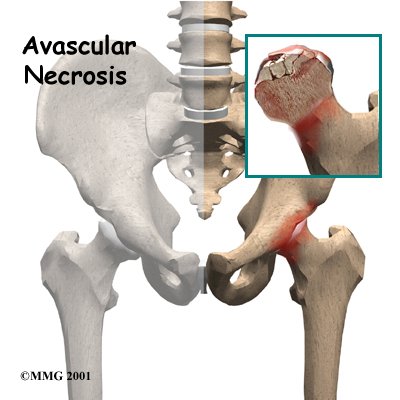
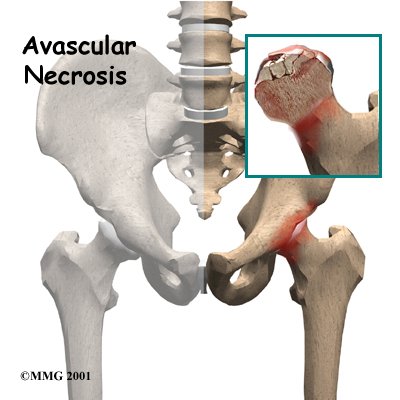 Bones are living tissue, and like all living tissues they rely on blood vessels to bring blood to keep them alive. Most living tissues have blood vessels that come from many directions into the tissue. If one blood vessel is damaged it may not cause problems, since there may be a backup blood supply coming in from a different direction. Certain joints of the body, however, have only a few blood vessels that bring in blood. One of these joints is the hip. This document will describe what happens when this blood supply is damaged and results in what is called avascular necrosis (AVN) of the hip. Another name for this condition is osteonecrosis (which means “bone death”).
Bones are living tissue, and like all living tissues they rely on blood vessels to bring blood to keep them alive. Most living tissues have blood vessels that come from many directions into the tissue. If one blood vessel is damaged it may not cause problems, since there may be a backup blood supply coming in from a different direction. Certain joints of the body, however, have only a few blood vessels that bring in blood. One of these joints is the hip. This document will describe what happens when this blood supply is damaged and results in what is called avascular necrosis (AVN) of the hip. Another name for this condition is osteonecrosis (which means “bone death”).
This guide will help you understand:
- how AVN develops
- how health care professionals diagnose this condition
- what treatments are available
- what Combined Therapy Specialties approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Hip Pain|limit:15|heading:Hear from some of our patients who we treated for *Hip Pain*#
Anatomy
Where does AVN develop?
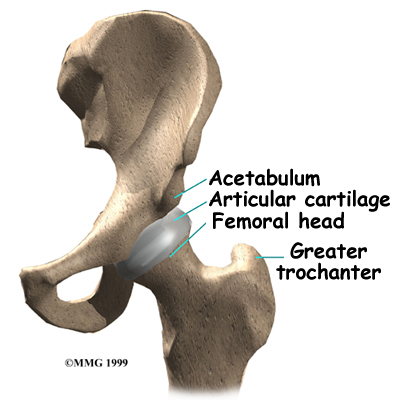
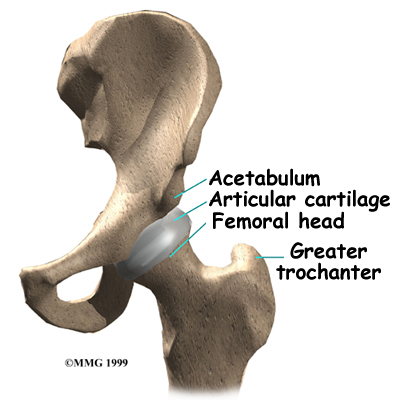
The hip joint is one of the true ball-and-socket joints of the body. The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone. The thighbone itself is called the femur, and the ball on the end is the femoral head. The ball and socket arrangement gives the hip the large amount of motion needed for daily activities such as walking, squatting, and climbing stairs. Thick muscles of the buttock at the back and the thigh in the front surround the hip.
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the surfaces to slide against one another without damage.
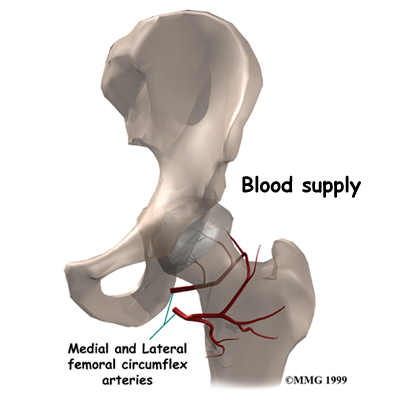
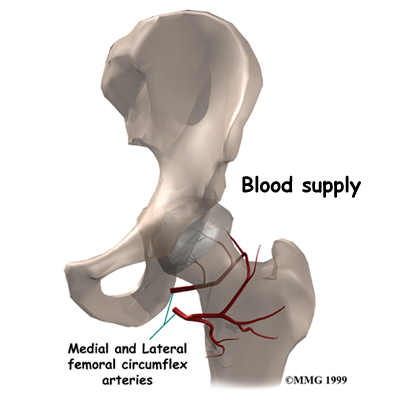
All of the blood supply comes into the ball that forms the hip joint through the neck of the femur (the femoral neck), a thinner area of bone that connects the ball to the shaft. If this blood supply is damaged, there is no backup. Damage to the blood supply can cause death of the bone that makes up the ball portion of the femur. Once this occurs, the bone is no longer able to maintain itself.
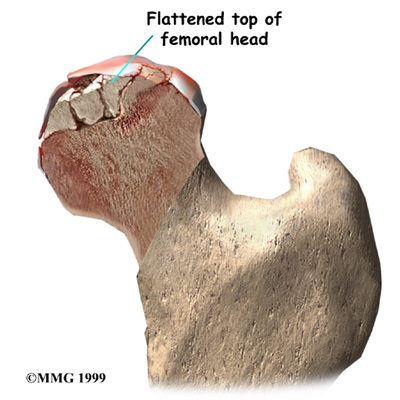
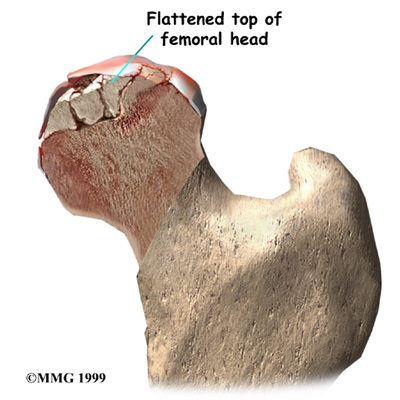 Living bone is always changing. To maintain a bone's strength, bone cells are constantly repairing the wear and tear that affects the bone tissue. If this process stops the bone can begin to weaken, just like rust can affect the metal structure of a bridge. Eventually, just like a rusty bridge, the bone structure begins to collapse.
Living bone is always changing. To maintain a bone's strength, bone cells are constantly repairing the wear and tear that affects the bone tissue. If this process stops the bone can begin to weaken, just like rust can affect the metal structure of a bridge. Eventually, just like a rusty bridge, the bone structure begins to collapse.
When AVN occurs in the hip joint, the top of the femoral head (the ball portion) collapses and begins to flatten. This occurs because this area is where most of the weight is concentrated. The flattening creates a situation where the ball no longer fits perfectly inside the socket. Like two parts of a mismatched piece of machinery, the joint begins to wear itself out. This leads to pain in the hip joint and eventually to osteoarthritis of the joint.
Related Document: Combined Therapy Specialtiess Guide to Osteoarthritis of the Hip
Related Document: Combined Therapy Specialtiess Guide to Hip Anatomy
Causes
Why do I have this problem?
There are many causes of AVN. Anything that damages the blood supply to the hip can cause AVN.
Injury to the hip itself can damage the blood vessels. Fractures of the femoral neck (the area connecting the ball of the hip joint) can damage the blood vessels. A dislocation of the hip out of the socket can tear the blood vessels. It usually takes several months for AVN to show up, and it can even become a problem up to two years following this type of injury.
Some medications are also known to cause AVN. Corticosteroids (cortisone) such as prednisone or methylprednisolone are the most common drugs known to lead to AVN. This is usually only a problem in patients who must take cortisone every day due to other diseases, such as advanced arthritis or to prevent rejection of an organ transplant.
Sometimes there is no choice, and cortisone has to be prescribed to treat a condition, knowing full well that AVN may occur. Local injection with cortisone, such as one or two injections into joints to treat arthritis or bursitis, has not been proven to cause AVN but some patients have developed AVN within the first month of taking these drugs orally (pills by mouth). Patients taking both corticosteroids and statin drugs (cholesterol-lowering medications) seem to have the greatest risk for developing AVN of the femoral head.
A clear link exists between AVN and lifestyle choices such as smoking and alcohol abuse. Smoking causes blood vessels to constrict or narrow thereby limiting the amount of blood flow to an area such as the hip with its already limited backup supply. Excessive alcohol intake somehow damages the blood vessels and can lead to AVN. Deep sea divers and miners who work under great atmospheric pressures are also at risk for damage to the blood vessels. The increased pressure at such depths causes tiny bubbles to form in the blood stream, which can block the blood vessels to the hip, damaging the blood supply.
There is a long list of other diseases and conditions that are associated with an increased incidence of femoral head osteonecrosis. These conditions are referred to as nontraumatic causes. For example, there is a link between osteonecrosis and problems like gout (hyperuricemia,) leukemia, sickle cell diseases, and HIV infection as well as a link with less well-known diseases such as Gaucher disease, and Caisson's disease.
Symptoms
What does AVN feel like?
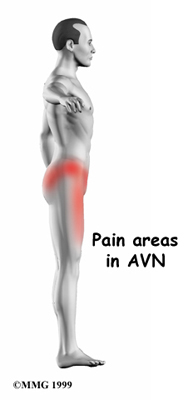
The first symptom of AVN is pain when weight is placed on the hip. The pain can be felt in the groin area, the buttock area, and down the front of the thigh. As the problem progresses, the symptoms include development of a limp when walking and stiffness in the hip joint. Eventually, the pain will also be present at rest and may even interfere with sleep.
Diagnosis
How do health care professionals identify this condition?
Diagnosis begins at Combined Therapy Specialties with a complete history and physical examination.
Your physical therapist will ask questions about where precisely your pain is, when the pain began, what you were doing when the pain started, and what movements aggravate or ease the pain. They will also want to know about your occupation, what other medical problems you have, and your medication use. In addition, if AVN is suspected, they may inquire about whether you drink alcohol or smoke.
Next your physical therapist will do a physical examination to determine exactly where your pain is, to assess how much stiffness you have in your hip joint, to determine if your hip is weak, and to assess whether or not you are walking with a limp. Your therapist will palpate, or touch, around the hip joint, including the buttocks and back areas, to determine where most of your pain is located. Your therapist will also move your hip into different positions to determine which motions cause or ease your discomfort. Finally, they will want to look at your foot position and alignment when you stand, and may ask you to walk or squat so alignment can be determined during these activities as well. If AVN is suspected your physical therapist will likely encourage X-rays to be done.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Investigations
X-rays will usually show AVN if it has been present for an extended period of time. In the very early stages, it may not show up on X-rays even though you are having pain. In the advanced stages, the hip joint will be very arthritic, and it may be hard to tell whether the main problem is AVN or advanced osteoarthritis of the hip. Either way, the treatment is basically the same.
If the X-rays fail to show AVN, you may need to have a bone scan done to determine if the pain in your hip is coming from early AVN. A bone scan involves injecting tracers into your blood stream firstly and then several hours later using a large camera to take a picture of the bone around the hip joint. If there is no blood supply to the femoral head, the picture will show a blank spot where the femoral head should be outlined on the film.
With today’s technology becoming more advanced, often these days a magnetic resonance image (MRI) is done instead of a bone scan. The MRI scan is probably the most common test used to look for AVN of the hip. The MRI scanner uses magnetic waves instead of radiation. Multiple pictures of the hip bones are taken by the MRI scanner. The images look like slices of the bones. The MRI scan is very sensitive and can show even small areas of damage to the blood supply of the hip, even just hours after the damage has occurred.
Your doctor or surgeon will use these imaging studies in order to plan the best treatment approach for you. He or she will look at where the damage has occurred, the size of any lesions, whether or not there has been any collapse of the bone, and determine if any arthritic changes have developed. Based on these findings, the condition will be classified as either mild, moderate, or severe.
Treatment
What can be done for the condition?
Once AVN has occurred, the treatment choices are determined by how far along the problem is and your symptoms. Other factors that guide treatment decisions include your age, activity level, general health including any specific health problems present, and your life expectancy. For example, patients with other serious health problems or with a limited life expectancy might be treated with nonoperative care. While the symptoms may be reduced with pain medications and anti-inflammatory medications, no medical treatments will restore the blood supply to the femoral head and reverse the AVN.
Nonsurgical Treatment
If AVN is caught early, non-surgical treatment may be an option. Nonsurgical treatment involves using medication as well as doing physical therapy at Combined Therapy Specialties.
In regards to medication, anti-inflammatories are often used to ease pain. Bisphosphonates are another group of medications that can be helpful. One particular bisphosphonate, Fosamax, which is normally used for the treatment of osteoporosis, has been shown effective in reducing the risk of femoral head collapse in patients with avascular necrosis. In some cases, surgeons also prescribe biophysical treatment modalities such as electrical stimulation or shock wave therapy in an attempt to get the bone to heal. Sometimes these measures may help delay the need for surgery, but they rarely reverse the problem.
Nonsurgical Rehabilitation
Physical therapy can be very effective in treating AVN of the femoral head if it is detected early. It can help to ease your pain and prevent further damage but again, treatment is not aimed to reverse the problem of damage has already been done. Early detection and treatment with physical therapy is the key to nonsurgical management of AVN.
During your first visit to Combined Therapy Specialties your physical therapist will take some baseline measurements in regards to your pain level, hip mobility, and your ability to do certain activities so that any improvement or regression over time can be measured. The first few treatments will focus on decreasing any pain or inflammation you may have. Ice is a very useful modality to reduce pain, however, many patients find heat to be more soothing and pain relieving in the case of the deep hip joint. Either one is appropriate depending on the relief it provides in your individual case. Your physical therapist may also use electrical modalities such as ultrasound or interferential current to decrease the pain and inflammation. Massage, particularly for the buttocks, back, or anterior and lateral hip muscles, may also be helpful.
Decreasing the load that the hip joint bears can be very effective in allowing the bone to heal as well as managing pain. This decreased load is achieved by having you use crutches or a walker instead of putting weight through your affected leg. If bearing no weight on the leg is too difficult, or deemed not completely necessary by your physical therapist, putting some weight through the leg, but bearing less than full body weight on that side can still be effective in giving the hip a chance to heal and in reducing your pain. Your physical therapist will teach you how to safely use the crutches or a walker. If you have stairs at home, they will also show you how to use the crutches on stairs to ensure that you are as mobile as possible while using them. Using the walking aid appropriately will avoid other problems in associated joints later on. Although helpful for your hip, unfortunately, putting no or only some weight on your leg and using a walking aid for too long, however, can have a detrimental effect on your muscles and joints, and will also cause compensatory problems elsewhere in the body, such as in your ankle, shoulders or back. The optimal amount of time to use a walking aid in order to positively affect AVN healing will be determined by your physical therapist in conjunction with advice from your doctor or surgeon.
Once you are no longer required to use a walking aid, your physical therapist will educate you on proper gait. We all take thousands of steps per day simply to walk around, so it is imperative that each step you take is done properly, without putting any excessive pressure through your healing hip joint. If you are unable to walk without a limp, your physical therapist may suggest that you continue to use a walking aid such as one crutch or a cane/stick, for a longer period of time.
In addition to pain relief, the main goals of physical therapy treatment at Combined Therapy Specialties are to avoid losing range of motion, to keep your hip and associated muscles strong, to avoid further injury, as well as to keep you doing as many of your regular functional activities as possible.
In order to achieve the range of motion goal your physical therapist at Combined Therapy Specialties will prescribe a series of stretching exercises that you will practice in the clinic and also do as part of a home exercise program. Maintaining range of motion is crucial to avoid further wear and tear on the hip joint. If the joint is not moving well into all ranges of motion, the joint surface does not get its required nutrition and more easily breaks down leading to early osteoarthritis. Moving the joint also helps to move any swelling that may be present, and gets fresh blood to the healing areas. Only mild discomfort at the very end ranges of motion during these stretching exercises, however, is permissible. Any sharp or moderate discomfort should be heeded as it means that too much pressure is being put on the delicate healing bone. An exercise bike can be very useful in order to gain range of motion. Even if you are unable to fully rotate the pedals of the bike, the forwards and backwards motion still assists the joint nutrition and aids in gaining range of motion. Stretches for your knee, ankle and calf may also be necessary as these areas can become tight with the use of a walking aid.
If necessary, and as healing allows, your physical therapist may mobilize your hip joint. This hands-on technique encourages the hip to move gradually into its normal range of motion. Mobilization of the hip may be combined with assisted stretching of any tight muscles around the joint. Again, the healing bone of the hip joint is delicate therefore anything more than mild discomfort at end ranges of motion should be strictly heeded.
Next your therapist will prescribe strengthening exercises. These exercises will focus on the muscles of your hip and thigh but will also include exercises for your back and core area as they play a large supporting role for your hips. Due to compensatory walking and movement patterns while you are in pain it is common to develop a muscular weakness in certain muscles around the hip, and an overall muscular imbalance.
Exercises that involve the entire lower limb, such as squats on both legs at the same time or just one leg, will be prescribed. Exercises that work the muscles while in standing most effectively assist with daily activities such as walking and stair climbing, however they also put the most amount of stress through the hip joint. Other exercises in sitting or lying, for this reason, may also be prescribed. Exercises in these non-weightbearing positions are excellent as they allow you to target specific muscles around the hip, such as the gluteals, even if you are not weightbearing on that side. Your therapist may use an electrical muscle stimulator to assist your muscles in contracting as you do your exercises; this will help you to more rapidly gain your strength back. Exercises may also include the use of Theraband or weights to provide some added resistance for your hip and lower extremity. If you have access to a pool, your therapist may suggest you go into the pool to do your exercises. The buoyancy and hydrostatic properties of the water along with the warmth of the water (provided it is a heated pool) can assist greatly in providing comfort to the hip joint and often allows you to exercise through greater ranges of motion and with less discomfort.
As a result of any injury the receptors in your joints and ligaments that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. A period of decreased mobility and reduced weight bearing will add to this decline. When balance and proprioception is declined, your joints and your limb as a whole will not function as efficiently and the decline may contribute to further injury in the future. For this reason a final component of our treatment at Combined Therapy Specialties will be to prescribe exercises for you to regain balance and proprioception. These exercises might include activities such as standing on one foot or balancing on an unstable surface such as a soft mat, or a soft plastic disc. More advanced exercises may involve side to side motions or even light hopping and jumping if your hip is healed enough to tolerate these activities.
During all of your exercises your physical therapist at Combined Therapy Specialties will pay particular attention to your exercise technique to ensure that you are not using any compensatory patterns or are developing bad habits in regards to how you use your hip and lower extremity. If you do not pay close attention to how you use your joint and limb once your pain has settled inefficient patterns that developed due to pain can become habitual, and compensatory pain can develop either in your hip or back, or another joint. In addition, poor movement patterns lead to faster wearing down of the hip joint socket, namely early osteoarthritis. Your physical therapist at Combined Therapy Specialties will be crucial to providing you with feedback regarding correcting old habitual patterns and developing new, efficient patterns during your daily activities.
As your range of motion, strength, and proprioception improve, your therapist will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows, and to incorporate exercises that simulate your specific everyday activities of daily living and any recreational activities that you may want to return to.
Asides from directly rehabilitating your hip, at Combined Therapy Specialties we also highly recommend maintaining the rest of your body’s fitness with regular exercise while your hip is improving. This exercise can be done simultaneously to your specific hip rehabilitation. You can use an upper body bike if you are unable to use a normal stationary cycle, or it may be permissible to do gentle aerobic exercises in a pool. A stationary bike is often the best cardiovascular activity once your range of motion and pain levels allow it. Weights for the upper extremities and other leg are also strongly encouraged. Advanced exercises such as the stepper or elliptical machines may be used once your hip has recovered to an acceptable level. Your physical therapist at Combined Therapy Specialties can provide a program and advice for you to maintain your general fitness while rehabilitating your hip.
When you are well under way, regular visits to our clinic will end. Your physical therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
As mentioned above, rehabilitation at Combined Therapy Specialties can assist a hip with AVN if the process isn’t too far advanced. If, however, your pain continues longer than it should or your therapy is not progressing as your physical therapist would expect, a surgical treatment option may be required.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Surgery
If the femoral head has not begun to collapse, your surgeon may suggest an operation to try to increase the blood supply to the femoral head. Several operations have been designed to do this.
Decompressing the Femoral Head
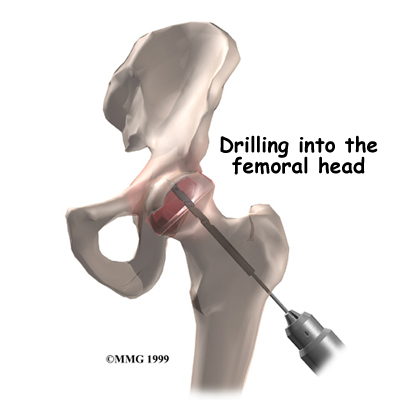
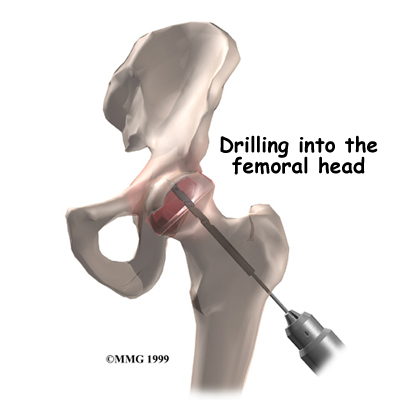 The simplest operation is to drill one or several holes through the femoral neck and into the femoral head, trying to reach the area that lacks blood supply. The drill bores out a plug of bone within the femoral head. This operation is thought to do two things: (1) it creates a channel for new blood vessels to quickly form into the area that lacks blood supply, and (2) it relieves some of the pressure inside the bone of the femoral head. Relieving this pressure seems to help decrease the pain patients experience from AVN.
The simplest operation is to drill one or several holes through the femoral neck and into the femoral head, trying to reach the area that lacks blood supply. The drill bores out a plug of bone within the femoral head. This operation is thought to do two things: (1) it creates a channel for new blood vessels to quickly form into the area that lacks blood supply, and (2) it relieves some of the pressure inside the bone of the femoral head. Relieving this pressure seems to help decrease the pain patients experience from AVN.
Decompression is often accompanied by the use of bone grafts with or without growth factors, a procedure designed to stimulate bone growth at the site of the defect. The donated bone comes from the patient (taken from the pelvic bone or lower leg). The bone is crushed up into tiny pieces and applied to the hole or defect caused by the necrotic process.
The decompression operation (with or without bone grafting) is done through a very small incision in the side of the thigh. The surgeon watches on a type of X-ray that shows the bones on a TV screen, called a fluoroscope, as a drill is used. The surgeon uses the fluoroscope to guide the drill where it needs to go. This operation is usually done as an outpatient procedure, and you will be able to go home with crutches the same day.
Fibular Bone Graft
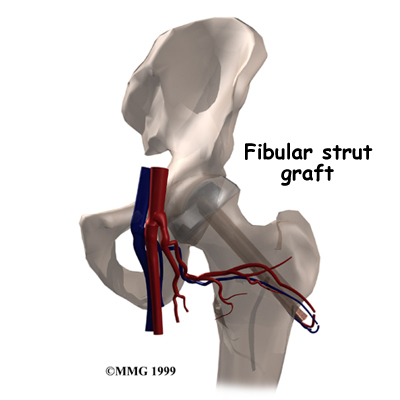
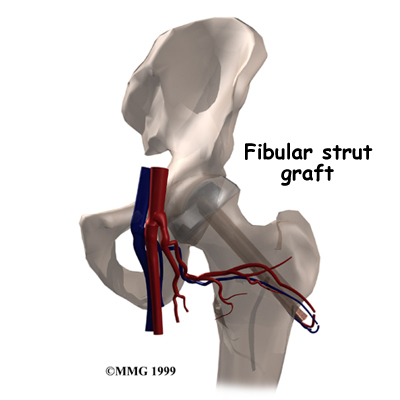 A more complicated procedure to try to increase the blood supply to the femoral head is a vascularized fibular bone graft procedure. This is actually a tissue transplant rather than a classic bone graft. With this procedure the graft is taken from the fibula, which is the thin bone that runs next to the shin bone. The surgeon removes a piece of the small bone from the fibula along with the blood vessels to the bone. The surgeon then drills a hole through the side of the femur and into the femoral head. The surgeon attaches the blood vessels from the fibula to one of the blood vessels around the hip. This creates instant blood flow into the bone graft and into the head of the femur. This operation does two things: (1) it brings blood flow to the femoral head through the bone graft, and (2) because the fibular bone graft is strong, it keeps the femoral head from collapsing as the bone heals itself. Being that the graft supports the femoral head, the graft is also referred to as a strut graft. This procedure is an inpatient procedure and will require you to stay in the hospital for several days. It is a very complicated operation and is not commonly done. It is not always successful because the blood supply to the graft is fragile and may not form completely.
A more complicated procedure to try to increase the blood supply to the femoral head is a vascularized fibular bone graft procedure. This is actually a tissue transplant rather than a classic bone graft. With this procedure the graft is taken from the fibula, which is the thin bone that runs next to the shin bone. The surgeon removes a piece of the small bone from the fibula along with the blood vessels to the bone. The surgeon then drills a hole through the side of the femur and into the femoral head. The surgeon attaches the blood vessels from the fibula to one of the blood vessels around the hip. This creates instant blood flow into the bone graft and into the head of the femur. This operation does two things: (1) it brings blood flow to the femoral head through the bone graft, and (2) because the fibular bone graft is strong, it keeps the femoral head from collapsing as the bone heals itself. Being that the graft supports the femoral head, the graft is also referred to as a strut graft. This procedure is an inpatient procedure and will require you to stay in the hospital for several days. It is a very complicated operation and is not commonly done. It is not always successful because the blood supply to the graft is fragile and may not form completely.
Rotational Osteotomy
In cases of small lesions involving less than one-third of the surface of the femoral head, performing a rotational osteotomy has been very successful. This procedure involves making a cut through the bone and turning the head of the femur so that the necrotic bone is no longer bearing any weight.
Artificial Hip Replacement
When AVN is in the advanced stages, the condition is no different from osteoarthritis of the hip joint. Your surgeon will probably recommend replacing the hip with an artificial hip joint. For those patients with a limited bone defect that only affects the femoral head and does not extend into the hip socket, a resurfacing procedure might be considered. Hip resurfacing arthroplasty is a type of hip replacement that replaces the arthritic surface of the joint but removes far less bone than the traditional total hip replacement.
Post-surgical Rehabilitation
The rehabilitation you will need after surgery for AVN depends entirely on what surgical procedure was performed. Obviously those procedures that are more complicated will require more intensive therapy at Combined Therapy Specialties for a longer period of time. You may even need to be seen by an inpatient physical therapist so you can start some exercises while you are still in the hospital.
After being discharged from the hospital you should begin physical therapy at Combined Therapy Specialties as soon as your surgeon allows. Some surgeons will recommend that you begin rehabilitation immediately, whereas others prefer that you wait until you are able to put a sufficient amount of weight through your surgical side.
After surgery for AVN you will be required to use a walking aid such as a walker or crutches. After a drilling operation, you will probably use the walker or crutches for six weeks or so. Due to the drill holes weakening the bone around the hip, fracturing the hip by putting too much weight on it is possible. Using a walking aid allows pressure to be taken off the bone while it heals and reduces the risk of fracturing your hip while the bone is healing. Patients who have had bone and blood vessels grafted are required to limit how much weight they place on the hip for up to six months.
If you are still using a walker or crutches by the time we first see you at Combined Therapy Specialties, your physical therapist will ensure you are using them safely, properly, and confidently while abiding by your weight bearing restrictions. With crutches we will ensure that you can safely use them on stairs. If you are no longer using a walking aid, or once you no longer need one, your physical therapist will focus on normal gait re-education to ensure that you are putting only the necessary forces through the surgical side with each step, and are not compensating in any way. Until you are able to walk without a significant limp, we recommend that you continue to use a walking aid, such as your crutches, or a cane/stick. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to use a walking aid until virtually normal walking can be achieved. Your Combined Therapy Specialties physical therapist will advise you, in conjunction with your surgeon’s protocol, regarding the appropriate time for you to be ambulating without any walking aid at all.
During your first few appointments at Combined Therapy Specialties your physical therapist will focus on relieving any pain and/or inflammation you may still have from the surgical procedure. They may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere down the extremity. In addition, your physical therapist may massage your hip, back, leg or ankle to improve circulation and help decrease your pain.
The next part of our treatment will focus on regaining the range of motion in your hip. Your physical therapist at Combined Therapy Specialties will prescribe a series of stretching exercises that you will practice in the clinic and also do as part of a home exercise program. You may experience a small amount of discomfort at the end ranges of motion initially, but despite this it is important to perform the range of motion exercises as prescribed because moving the joint also helps to move the swelling, get fresh blood to the healing areas, and provides nutrition to the joint. Only mild discomfort, however, is permissible. Any sharp or moderate discomfort should be heeded. An exercise bike at this stage of recovery can be very useful. Even if you are unable to fully rotate the pedals of the bike, the forwards and backwards motion still assists the joint nutrition and aids in gaining range of motion. Stretches for your knee, ankle and calf may also be necessary as these areas can become tight with the use of a walking aid.
If necessary, and as time and healing allows, your physical therapist may mobilize your hip joint. This hands-on technique encourages the hip to move gradually into its normal range of motion. Mobilization of the hip may be combined with assisted stretching of any tight muscles around the surgical site.
Strengthening exercises are another important component of your post-surgical rehabilitation. Due to compensatory walking and movement patterns in response to pain it is common to develop a muscular weakness in certain muscles around the hip, and an overall muscular imbalance. Exercises will focus mainly on the muscles of your hip and thigh but your therapist will also include exercises for your back and core areas as they play a large supporting role for your hips. Exercises that involve the entire lower limb, such as squats on both legs at the same time, or just on one leg, will be prescribed. Exercises that work the muscles while in standing are most effective for improving daily activities such as walking and stair climbing. Other exercises in sitting or lying, however, may also be prescribed. Exercises in these non-weightbearing positions are excellent as they allow you to target specific muscles around the hip, such as the gluteals, even if you are not weightbearing on that side. Your therapist may use an electrical muscle stimulator to assist your muscles in contracting as you do your exercises; this will help you to more rapidly gain your strength back. Exercises may also include the use of Theraband or weights to provide some added resistance for your hip and lower extremity. If you have access to a pool, your therapist may suggest you go to the pool to do your exercises. As mentioned above, the buoyancy and hydrostatic properties of the water along with the warmth of the water (provided it is a heated pool) can assist greatly in providing comfort to the hip joint and often allows you to exercise within a greater range of motion.
As a result of any injury or surgery, the receptors in your joints and ligaments that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. A period of decreased mobility and reduced weight bearing will add to this decline. When balance and proprioception has declined, your joints and your limb as a whole do not function as efficiently, and the decline may contribute to further injury in the future. Once you are able to put full weight onto your surgical side a final component of our treatment at Combined Therapy Specialties will be to prescribe exercises for you to regain this balance and proprioception. These exercises might include activities such as standing on one foot or balancing on an unstable surface such as a soft mat, or a soft plastic disc.
During all of your exercises your physical therapist at Combined Therapy Specialties will pay particular attention to your exercise technique to ensure that you are not using any compensatory patterns or are developing bad habits in regards to how you use your hip and lower extremity. If you do not pay close attention to how you use your joint and limb post-surgically inefficient patterns that developed due to pain even prior to surgery can remain as habits and compensatory pain can develop either in your hip or back, or another joint. In addition, poor movement patterns lead to faster wearing down of the hip joint socket, namely early osteoarthritis. Your physical therapist at Combined Therapy Specialties will be crucial to providing you with feedback regarding correcting poor movement patterns and developing new, efficient patterns during your daily activities.
As your range of motion, strength, and proprioception improve, your therapist will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows, and to incorporate exercises that simulate your specific everyday activities of daily living and any recreational activities that you may want to return to. If you are still very active, heavy sports that require running, jumping, quick stopping and starting, and cutting may need to be limited depending on the state of your hip joint, and which surgical procedure has been performed. Your surgeon will advise you regarding which activities in your individual case are discouraged or not at all permissible.
Asides from directly rehabilitating the hip after surgery, at Combined Therapy Specialties we also highly recommend maintaining the rest of your body’s fitness with regular exercise while your hip is recovering. This exercise can begin very early post-surgically. You can use an upper body bike if you are not yet able to use a normal stationary cycle, or you may even be allowed to do gentle aerobic exercises in a pool. A stationary bike is often the best cardiovascular activity once your range of motion and pain levels allow it. Weights for the upper extremities and other leg are also strongly encouraged. Advanced exercises such as the stepper or elliptical machines may be used once your hip has recovered to an acceptable level. Your physical therapist at Combined Therapy Specialties can provide a program and advice for you to maintain your general fitness while you recover from your surgery
When you are well under way, regular visits to our clinic will end. Your physical therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Generally the rehabilitation after surgery for AVN responds very well to the physical therapy we provide at Combined Therapy Specialties. If for some reason, however, your pain continues longer than it should or your therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon to confirm that the hip is tolerating the rehabilitation well and to ensure that there are no complications that may be impeding your recovery.
Portions of this document copyright MMG, LLC.
Combined Therapy Specialties provides services for physical therapy in Asheville.
 Bones are living tissue, and like all living tissues they rely on blood vessels to bring blood to keep them alive. Most living tissues have blood vessels that come from many directions into the tissue. If one blood vessel is damaged it may not cause problems, since there may be a backup blood supply coming in from a different direction. Certain joints of the body, however, have only a few blood vessels that bring in blood. One of these joints is the hip. This document will describe what happens when this blood supply is damaged and results in what is called avascular necrosis (AVN) of the hip. Another name for this condition is osteonecrosis (which means “bone death”).
Bones are living tissue, and like all living tissues they rely on blood vessels to bring blood to keep them alive. Most living tissues have blood vessels that come from many directions into the tissue. If one blood vessel is damaged it may not cause problems, since there may be a backup blood supply coming in from a different direction. Certain joints of the body, however, have only a few blood vessels that bring in blood. One of these joints is the hip. This document will describe what happens when this blood supply is damaged and results in what is called avascular necrosis (AVN) of the hip. Another name for this condition is osteonecrosis (which means “bone death”).






 Living bone is always changing. To maintain a bone's strength, bone cells are constantly repairing the wear and tear that affects the bone tissue. If this process stops the bone can begin to weaken, just like rust can affect the metal structure of a bridge. Eventually, just like a rusty bridge, the bone structure begins to collapse.
Living bone is always changing. To maintain a bone's strength, bone cells are constantly repairing the wear and tear that affects the bone tissue. If this process stops the bone can begin to weaken, just like rust can affect the metal structure of a bridge. Eventually, just like a rusty bridge, the bone structure begins to collapse.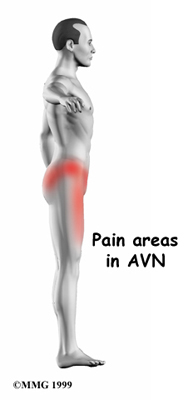
 The simplest operation is to drill one or several holes through the femoral neck and into the femoral head, trying to reach the area that lacks blood supply. The drill bores out a plug of bone within the femoral head. This operation is thought to do two things: (1) it creates a channel for new blood vessels to quickly form into the area that lacks blood supply, and (2) it relieves some of the pressure inside the bone of the femoral head. Relieving this pressure seems to help decrease the pain patients experience from AVN.
The simplest operation is to drill one or several holes through the femoral neck and into the femoral head, trying to reach the area that lacks blood supply. The drill bores out a plug of bone within the femoral head. This operation is thought to do two things: (1) it creates a channel for new blood vessels to quickly form into the area that lacks blood supply, and (2) it relieves some of the pressure inside the bone of the femoral head. Relieving this pressure seems to help decrease the pain patients experience from AVN.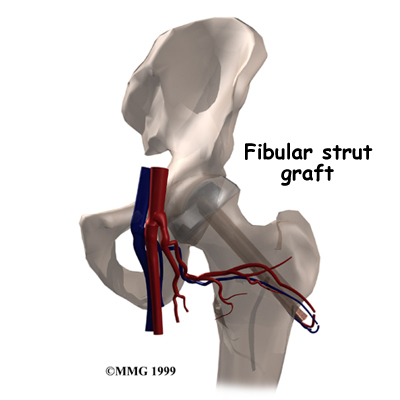 A more complicated procedure to try to increase the blood supply to the femoral head is a vascularized fibular bone graft procedure. This is actually a tissue transplant rather than a classic bone graft. With this procedure the graft is taken from the fibula, which is the thin bone that runs next to the shin bone. The surgeon removes a piece of the small bone from the fibula along with the blood vessels to the bone. The surgeon then drills a hole through the side of the femur and into the femoral head. The surgeon attaches the blood vessels from the fibula to one of the blood vessels around the hip. This creates instant blood flow into the bone graft and into the head of the femur. This operation does two things: (1) it brings blood flow to the femoral head through the bone graft, and (2) because the fibular bone graft is strong, it keeps the femoral head from collapsing as the bone heals itself. Being that the graft supports the femoral head, the graft is also referred to as a strut graft. This procedure is an inpatient procedure and will require you to stay in the hospital for several days. It is a very complicated operation and is not commonly done. It is not always successful because the blood supply to the graft is fragile and may not form completely.
A more complicated procedure to try to increase the blood supply to the femoral head is a vascularized fibular bone graft procedure. This is actually a tissue transplant rather than a classic bone graft. With this procedure the graft is taken from the fibula, which is the thin bone that runs next to the shin bone. The surgeon removes a piece of the small bone from the fibula along with the blood vessels to the bone. The surgeon then drills a hole through the side of the femur and into the femoral head. The surgeon attaches the blood vessels from the fibula to one of the blood vessels around the hip. This creates instant blood flow into the bone graft and into the head of the femur. This operation does two things: (1) it brings blood flow to the femoral head through the bone graft, and (2) because the fibular bone graft is strong, it keeps the femoral head from collapsing as the bone heals itself. Being that the graft supports the femoral head, the graft is also referred to as a strut graft. This procedure is an inpatient procedure and will require you to stay in the hospital for several days. It is a very complicated operation and is not commonly done. It is not always successful because the blood supply to the graft is fragile and may not form completely.
