Introduction
Physical therapy in Asheville for Elbow
Welcome to Combined Therapy Specialties patient resource about Unilateral Ligament Reconstruction.
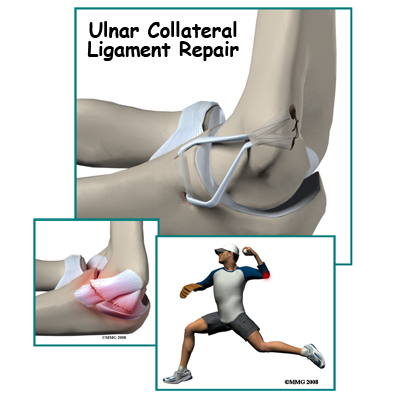
The doctors call it a UCLR ulnar collateral ligament reconstruction. Baseball players and fans call it Tommy John surgery -- named after the pitcher (Los Angeles Dodgers) who was the first to have the surgery in 1974. It is one of the major advancements in sports medicine in the last quarter century.
This guide will help you understand:
- what your surgeon hopes to achieve
- how do I prepare for this procedure
- what happens during the procedure
- what to expect as you recover
Anatomy
What’s the normal anatomy of the elbow?
The bones of the elbow are the humerus (the upper arm bone), the ulna (the larger bone of the forearm, on the opposite side of the thumb), and the radius (the smaller bone of the forearm on the same side as the thumb).
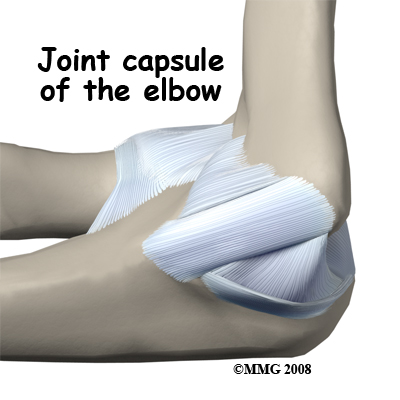
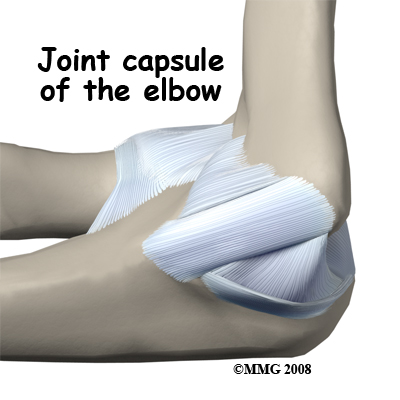
There are several important ligaments in the elbow. Ligaments are soft tissue structures that connect bones to bones. The ligaments around a joint usually combine together to form a joint capsule. A joint capsule is a watertight sac that surrounds a joint and contains lubricating fluid called synovial fluid.
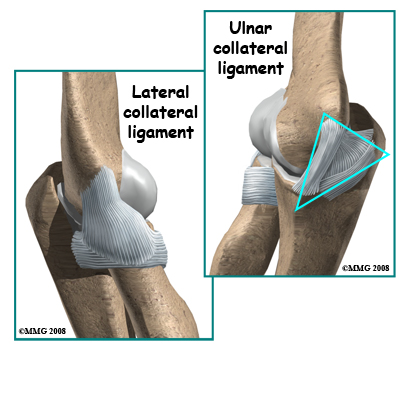
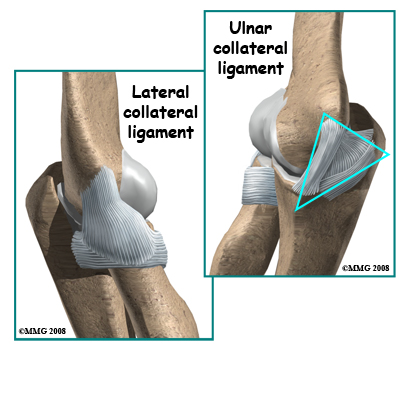
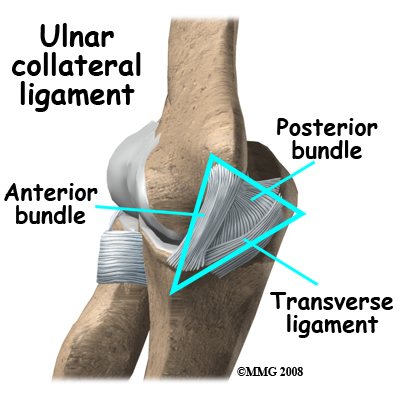
In the elbow, two of the most important ligaments are the ulnar collateral ligament (UCL) and the lateral collateral ligament. The UCL is also known as the medial collateral ligament. The ulnar collateral ligament is on the medial (the side of the elbow that's next to the body) side of the elbow and the lateral collateral is on the outside. The ulnar collateral ligament is a thick band of ligamentous tissue that forms a triangular shape along the medial elbow. It has an anterior bundle, posterior bundle, and a thinner, transverse ligament.
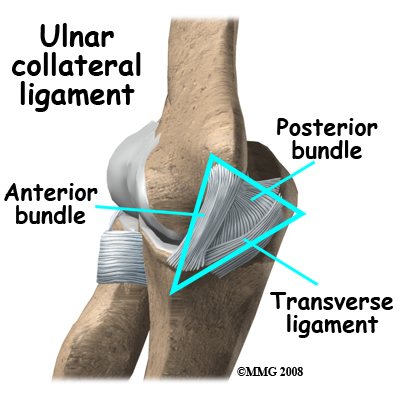
Together these two ligaments, the ulnar (or medial) collateral and the lateral collateral, connect the humerus to the ulna and keep it tightly in place as it slides through the groove at the end of the humerus. These ligaments are the main source of stability for the elbow. They can be torn when there is an injury or dislocation of the elbow. If they do not heal correctly the elbow can be too loose or unstable. The ulnar collateral ligament can also be damaged by overuse and repetitive stress, such as the throwing motion.
Related Document: Combined Therapy Specialties to Elbow Anatomy
Elbow Anatomy Introduction
Rationale
What does my surgeon hope to achieve?
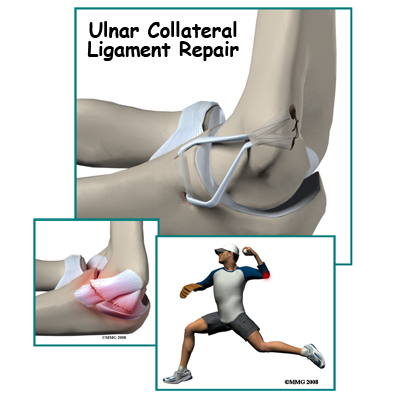
Surgical treatment is designed to restore medial stability of the elbow. Full return to previous activities is the main goal. This is especially true for those athletes who want to remain active and competitive in sports. Many throwing athletes who develop this condition have pain in the elbow during and after throwing activities. They may also develop numbness and tingling in the hand due to stretching of the ulnar nerve at the elbow. Successful treatment of the condition should improve or eliminate these symptoms.
Who can benefit from this procedure?
Throwing athletes (especially baseball pitchers) at the college and professional level are affected most often by this injury requiring surgery. Minor league athletes and younger sports participants may also develop this injury requiring surgical care. Anyone with this injury who has not benefitted (gotten better) with conservative care is a candidate for surgery.
Preparation
How should I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You need to understand as much about the procedure as possible. If you have concerns or questions, you should talk to your surgeon.
Once you decide on surgery, you need to take several steps. Your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
What happens during the operation?
Reconstruction
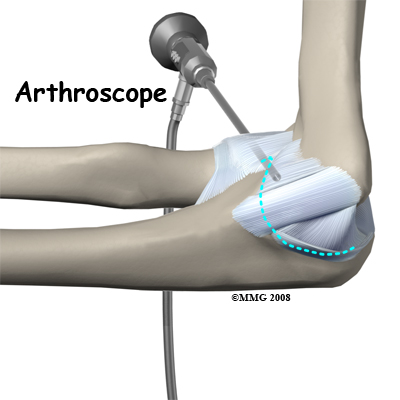
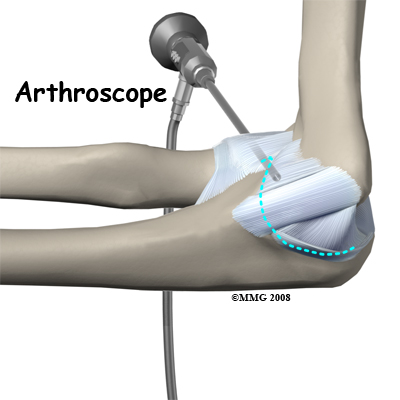
If you are having problems that may be coming from inside the joint, such as arthritis and loose bodies, your surgeon may perform an arthroscopy before the actual reconstruction procedure is done. During this procedure, a small TV camera is inserted into the elbow joint through two or three small (1/4 inch) incisions. Using special instruments your surgeon will be able to evaluate the joint, remove any loose bodies and bone spurs that may be causing problems. Arthroscopy is not always necessary.
 The reconstruction is performed though an on the medial (inside) side of the elbow joint. The damaged ulnar collateral ligament along the medial (inside) of the elbow is replaced with a tendon harvested from somewhere else in the body. The tendon graft can come from the patient's own forearm, hamstring, knee, or foot. This is called an autograft.
The reconstruction is performed though an on the medial (inside) side of the elbow joint. The damaged ulnar collateral ligament along the medial (inside) of the elbow is replaced with a tendon harvested from somewhere else in the body. The tendon graft can come from the patient's own forearm, hamstring, knee, or foot. This is called an autograft.
Over the years the way that surgeons perform this operation has improved. In the early days, the muscles on the inside of the elbow joint and forearm (the flexor muscles) were completely detached from the humerus and the ulnar nerve was re-routed from its normal position in the cubital tunnel on the back side of the elbow. This was done to be able to see the joint and protect the nerve. As surgeons have understood this problem more completely, these two parts of the operation have been eliminated. Now, the flexor muscles are not detached, but are split and retracted to allow the surgeon to see the areas of the elbow joint required to perform the operation successfully. The ulnar nerve is re-routed only if the patient is having symptoms of ulnar nerve damage before the operation is performed. These improvements have resulted in a less invasive procedure with a decreased rate of complications.
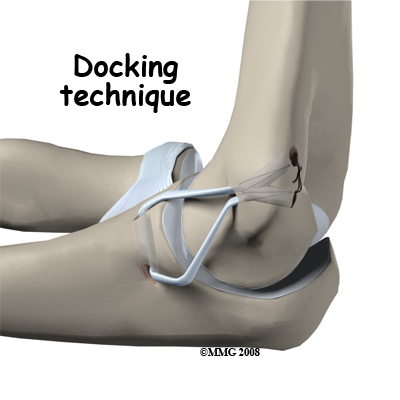
One common technique used to replace the damaged ulnar collateral ligament is called the docking technique. The surgeon drills two holes in the ulna and three in the medial epicondyle ( the small bump of bone on the inside of the elbow at the end of the humerus). The two holes in the ulna form a tunnel that the tendon graft will be looped through. The three holes in the medial epicondyle form a triangle. The bottom hole will be bigger than the top two holes, so that the surgeon can slide the end of the tendon graft into the bottom hole. The two top holes are used to pull the tendon graft into the tunnel using sutures that are attached to the graft and threaded through the two holes.
After the tendon is harvested, sutures are attached to both ends. The tendon is looped through the lower tunnel formed in the ulna, and stretched across the elbow joint. The two sutures attached to the ends of the graft are threaded into the larger bottom tunnel in the medial epicondyle and each is threaded out one of the upper, smaller holes.
 Using these two sutures, the surgeon pulls the end of the graft farther into the upper tunnel until the amount of tension is correct to hold the joint in position. The surgeon carefully puts the elbow through its full arc of motion and readjusts the tension on the sutures until he is satisfied that the proper ligamentous tension is restored. The two sutures are tied together to hold the tendon graft in that position.
Using these two sutures, the surgeon pulls the end of the graft farther into the upper tunnel until the amount of tension is correct to hold the joint in position. The surgeon carefully puts the elbow through its full arc of motion and readjusts the tension on the sutures until he is satisfied that the proper ligamentous tension is restored. The two sutures are tied together to hold the tendon graft in that position.
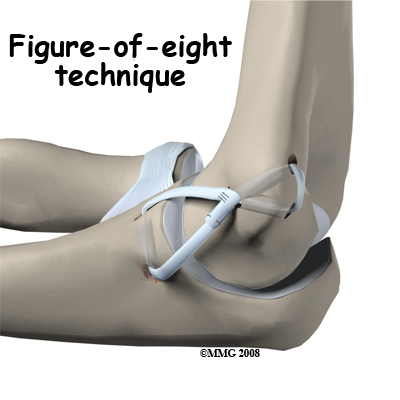
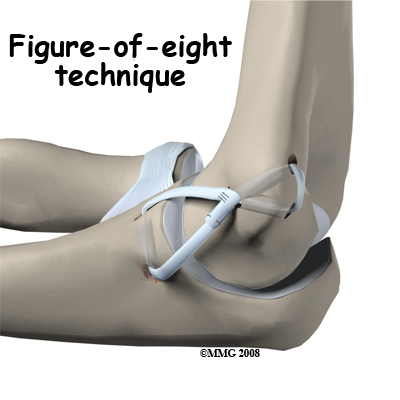
Another common technique to reconstruct the ulnar collateral ligament is the technique. In this technique, the tendon graft is threaded through two pairs of holes - two drilled in the medial epicondye and two in the ulna. The graft is looped through the holes in a figure of eight fashion. The two ends of the tendon are sutured to the tendon itself.
If there is any concern that the ulnar nerve has been stretched and damaged due to the instability (as mentioned above), it may be re-routed so that it runs in front of the elbow joint rather than through the cubital tunnel in the back of the elbow. The incision is sutured together and the elbow is placed in a large bandage and splint.
There are several newer techniques being developed that hopefully will make the procedure even less invasive while retaining the success that the docking technique has enjoyed.
Complications
What might go wrong?
As with all surgical procedures, complications can occur. This topic doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications are:
- anesthesia complications
- infection
- nerve or blood vessel damage
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Any operation carries a small risk of infection. You may be given antibiotics before the operation to reduce the risk of infection. If an infection occurs, you will most likely need more antibiotics to cure it.
Nerve or Blood Vessel Damage
Because the operation is performed so close to the nerves and vessels, it is possible to injure them during surgery. All of the nerves that travel down the arm pass across the elbow. The ulnar nerve is especially at risk for damage. Problems such as pain, numbness, and weakness in the arm and hand can be the consequences of nerve scarring, entrapment, or traction injury from the original trauma or from the procedure.
This condition is called a neuropathy. It may be temporary with gradual resolution of symptoms over a period of many months. If it doesn't resolve on its own or with physical therapy, further surgery may be needed. In a small number of cases, this complication is permanent.
Studies show that up to half of the patients treated by ligament reconstruction are left with a loss of full motion. The main problem is a five to 10 degree loss of extension (the elbow doesn't straighten all the way). This deformity does not affect strength or function. Earlier, more aggressive rehab may restore motion but at the risk of impaired healing of the graft.
Long-term complications can include chronic pain with throwing and chronic instability of the elbow.
After Surgery
What should I expect as I recover?
Repair or Reconstruction
The postoperative program is the same for repairs or reconstruction. At first your arm will be immobilized in a bulky dressing and a posterior splint for the first 10 days. It holds the elbow in a position of 90 degrees of flexion and neutral forearm rotation while leaving the wrist free to move. If non-absorbable sutures are used to close the incision, you may need these removed in 10 days.
You'll have about a four-inch long incision along the inside of your elbow. There may be some discomfort after surgery. Your surgeon can give you pain medicine to control the discomfort. You should keep your elbow elevated above the level of your heart for several days to avoid swelling and throbbing. Keep your elbow propped up on a stack of pillows when sleeping or sitting.
Portions of this document copyright MMG, LLC.
Our Treatment
Post-surgical Rehabilitation
What should I expect during my rehabilitation?
When you begin your Combined Therapy Specialties recovery program, we will start your rehabilitation with gentle handgrip, and shoulder and wrist mobilization exercises. Postoperative immobilization is usually discontinued in seven to 10 days at which time we will have you begin an active range of motion for the elbow. During this early stage of rehabilitation, our physical therapist may advise that you to wear a special hinged brace to protect the elbow.
We will instruct you in the active range of motion exercises to be done daily. Strengthening exercises for the entire upper quadrant (shoulder, arm, wrist, and hand) are also included in the post-operative program. Although the speed of recovery varies among individuals, specific strengthening exercises to help an athlete prepare for his or her particular sport usually begin around four months post-op. Up until this time, any stress to the medial elbow is avoided.
With careful adherence to our rehab program and completing the exercises daily, pitchers can often get their full range of motion back in six to eight weeks. As you continue with your Combined Therapy Specialties rehabilitation, we will progress to strength training with weight exercises. For the next four months, we will increase the weight used and start doing exercises that emphasize all parts of the arm.
Flexibility, conditioning, coordination, and strengthening are part of the daily program. You may use ice after throwing sessions to help control inflammation. We will use plyometric exercises throughout the training period. An aerobic portion of the exercise program is also advised to help the athlete return to sports at the same level (or even higher level) as before the surgery. Good, overall physical condition is important to prevent injury as the athlete returns to sports activity.
At times in your rehab and recovery, you may find it necessary to move back to a previous level of training if symptoms of pain and swelling recur. Your Combined Therapy Specialties physical therapist will guide you through the advancement (and regression) of your program. Additional training to restore normal joint proprioception (sense of joint position) and proper throwing mechanics is also provided.
Based on long-term studies of athletes over the years, the chances of a complete recovery after surgery are estimated at 85 to 90 percent. The process of rehabilitation to return to a level of playing equal to before the injury takes about a year for pitchers and about six months for position players.
The most often used criteria for resuming full (competitive) sports participation include 1) no pain with throwing, 2) full shoulder and elbow range of motion, 3) normal forearm strength, and 4) good throwing biomechanics.
Combined Therapy Specialties provides services for physical therapy in Asheville.







 The reconstruction is performed though an
The reconstruction is performed though an 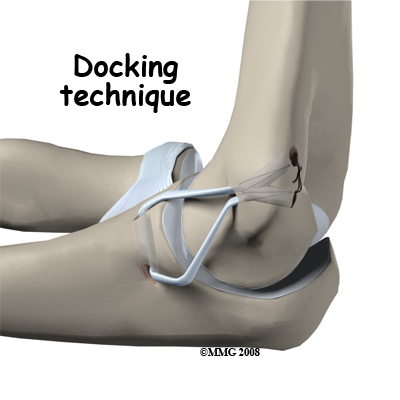
 Using these two sutures, the surgeon pulls the end of the graft farther into the upper tunnel until the amount of tension is correct to hold the joint in position. The surgeon carefully puts the elbow through its full arc of motion and readjusts the tension on the sutures until he is satisfied that the proper ligamentous tension is restored. The two sutures are tied together to hold the tendon graft in that position.
Using these two sutures, the surgeon pulls the end of the graft farther into the upper tunnel until the amount of tension is correct to hold the joint in position. The surgeon carefully puts the elbow through its full arc of motion and readjusts the tension on the sutures until he is satisfied that the proper ligamentous tension is restored. The two sutures are tied together to hold the tendon graft in that position.
