Introduction
Welcome to Combined Therapy Specialties guide to fractures of the forearm.
Forearm fractures are those that occur in the middle section (shaft) of the forearm bones. The forearm has a complex anatomy to serve its functions of supporting and positioning the hand in space and providing anchorage for muscles that serve hand function. To fully restore these functions after a forearm fracture the bones must heal in the normal anatomical position.
This guide will help you understand:
- what parts of the forearm are involved
- what the symptoms are
- what can cause these fractures
- how health care professionals diagnose these fractures
- what the treatment options are
- what Combined Therapy Specialties approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Elbow Pain|limit:15|heading:Hear from some of our patients who we treated for *Elbow Pain*#
Anatomy
What structures are most commonly injured?
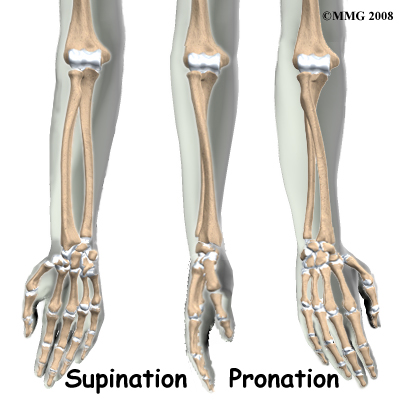
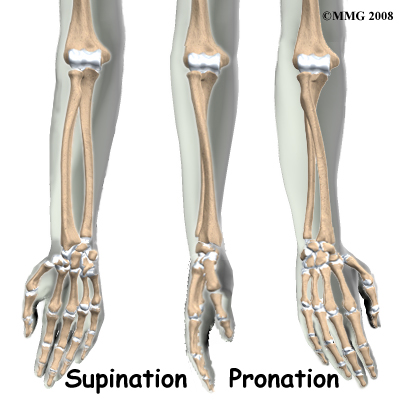
There are two bones in the forearm. The ulna is a straight thin bone that goes from the elbow to the wrist and forms the axis of rotation of the forearm. The radius is thin at one end becoming thicker and stronger towards the wrist. It is slightly bowed to allow it to rotate around the ulna when the forearm is rotated. To demonstrate this, place your forearm flat on a table in front of you with the palm up and the back of the little finger touching the table. Now roll the hand over until it is positioned palm down on the table. Note that the little finger and the elbow are still in nearly the same position while the thumb has moved from outside to inside. When the forearm rotates, the little finger side where the ulna is forms the axis (spindle) around which the rest of the forearm rotates. We can see that the radius is on the outside of the forearm when it is rolled outwards but crosses over the ulna when the forearm is rotated in. The radius is bowed to allow this movement to occur. If the bowing is not accurately restored after a fracture the forearm will not rotate correctly and this would limit some important functions of the hand.
Related Document: Combined Therapy Specialties Guide to Elbow Anatomy
Elbow Anatomy Introduction
Causes
How do fractures of the forearm commonly happen?
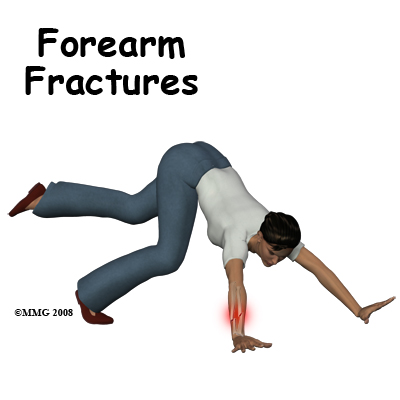
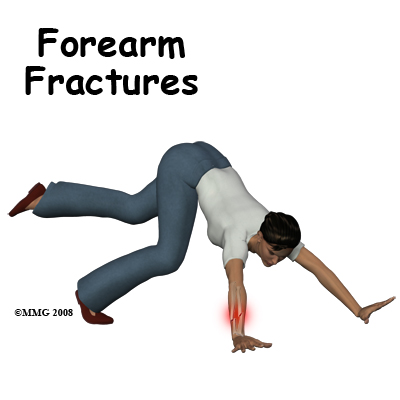
All fractures occur when the limb is subjected to stress outside the normal range. Forearm fractures most commonly occur in three situations- a blow to the forearm, a bending force such as falling on the outstretched hand, or a twisting force where the forearm is over-rotated. Most often these forces cause both bones to break, but a fracture of the ulna alone can occur if you put your arm up to ward off an attack. This isolated fracture of the ulna used to be called the nightstick fracture! Nowadays, the pattern is more common in sports collisions, motor vehicle accidents (MVAs), and falls but it does still occur with violent assault.
Twisting and bending fractures occur with falls, sports accidents, and MVAs. As with all fractures, the damage done to the muscles and tendons is a significant feature of the injury. Open fractures, where the bone comes out through the skin are quite common in the forearm.
Symptoms
What symptoms do forearm fractures cause?
Pain and tenderness immediately following an accident are the most common symptoms of a fractured forearm. The pain is made worse if the forearm is moved or rotated and may be partly relieved by splinting the limb. Deformity of the forearm is common following this type of fracture and there is immediate loss of hand function. You can no longer lift things or grip them with any strength. The forearm is often bruised and swollen. In some severe injuries there may be a wound where the broken bone end has come through the skin. Numbness of the hand is an indication that a nerve to the hand may have been injured at the time of the fracture.
Diagnosis
How will my fracture be evaluated?
First aid evaluation consists of inspecting the limb. A fracture would be assumed if the limb is severely painful, if the hand cannot be moved, or the forearm rotated or if the limb is deformed. A sling is usually a sufficient splint for transport to hospital.
In the Emergency Room assessment will include establishing the history and mechanism of injury, looking at the arm (inspection), and palpation (gently feeling it) for tender points. X-ray examination will be undertaken if there is suspicion of fracture of the forearm. In most situations an orthopedic surgeon will be consulted if a forearm fracture is confirmed by x-ray. The orthopedic evaluation will focus on the anatomy of the fracture, the patient's expectations, and a plan for treatment. There are no special tests usually employed in this situation, other than x-ray.
Our Treatment
What treatments should I consider?
Nonsurgical Treatment
An isolated fracture of the ulna (nightstick fracture,) may be treated in a cast. It is not as important to make the bone absolutely straight so the result of non-operative treatment is often acceptable. The arm is placed in a cast extending from the palm of the hand to above the elbow. This is called a long arm cast. The wrist is held in the neutral position and the elbow at 90 degrees of flexion. It may be painful to put on this cast so an anesthetic may be required for cast application.
For reasons described earlier, a fracture of both forearm bones needs to heal with great accuracy. Closed reduction, in which the bone ends are re-aligned without surgery is often not accurate enough. However, in some circumstances a closed reduction is tried. If this is successful the arm will be immobilized in a long arm cast. There is a risk that the fracture will displace in the cast, so frequent follow-up X-rays will be needed.
Surgery
If the ulna shaft fracture is badly displaced the forearm may need surgery to realign the bone fragments and to fixate them in place. This has the additional advantage of allowing early movement of the limb.
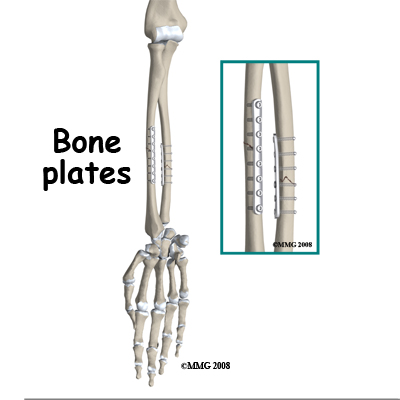
In the majority of cases, the surgeon will recommend surgery to ensure that the fracture is reduced accurately and fixed with internal fixation. Fixation with plates and screws is a common method although some surgeons recommend the less invasive method of placing a rod into the hollow medullary cavity of the bone, called intramedullary fixation.
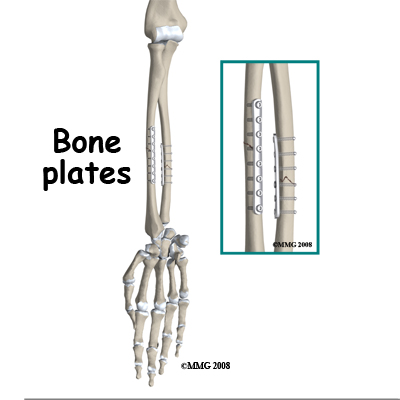
Because fixation allows early recovery of movement of the forearm and hand, the long-term risk of stiffness and loss of function are reduced. After surgery (internal fixation) a cast is not usually necessary although weight should not be put through the limb until the bone is healed. A sling for protection and pain relief is the usual practice but unloaded hand, wrist, and elbow movements can be started right away.
Removal of the implants is controversial. The hardware is often uncomfortable and in those cases the patient and surgeon usually agree to removal. However, about 1/10th of these cases have a re-fracture within six weeks of the removal operation. This risk deters some surgeons from removal of the hardware where there are no symptoms. Others believe that the life time risk of a problem from a retained plate is great enough to warrant removal of plates as a precaution.
Bone Healing
New bone formation (hard callus) is commonly seen on x-ray bridging across the fracture by six weeks. At this stage the fracture will not easily move out of position. If a cast was used it may be taken off at this stage. The decision to proceed is based on interpretation of the x-rays and assessment of the stage of healing reached.
Rehabilitation
If your fracture has been immobilized by a cast, then treatment with a physical therapist at Combined Therapy Specialties can begin once the cast is removed. While you are in the cast simple finger movements as well as exercises to maintain your shoulder range of motion, such as lifting your arm overhead, will be your only exercises.
If you have had surgery to fixate your forearm fracture, then rehabilitation at Combined Therapy Specialties will begin as soon as your surgeon recommends it. Each surgeon will set his or her own specific restrictions based on the type of fracture, surgical procedure used, personal experience, and whether the fracture is healing as expected. Generally, however, early non-weight bearing hand, wrist, and elbow movements will be allowed. Your physical therapist at Combined Therapy Specialties will prescribe these exercises for you and liaise with your surgeon regarding the optimal time to begin more advanced exercises such as putting weight through the healed forearm bone via the hand.
Even if extensive physical therapy for your forearm is not yet appropriate, at Combined Therapy Specialties we highly recommend maintaining the rest of your body’s fitness with regular exercise. Maintaining general cardiovascular fitness is easy with lower extremity fitness activities such as walking or using a stationary bike or stepper machine. Avid runners may even be able to continue running with clearance from the surgeon. Weights or weight machines for your lower extremity and opposite arm are also acceptable to use as long as the restrictions regarding your healing forearm are strictly abided by. Generally, lifting any weight with your injured limb will not be allowed or will be difficult as your forearm heals so you may require a friend to assist you with your workout setup if you are keen to continue while your bone heals. Your physical therapist can discuss the most appropriate way for you to maintain your fitness while abiding by your surgeon’s restrictions and can provide a general fitness program specific to your needs.
When the initial cast is removed or immediately after surgery, you may experience some pain when you start to move your wrist, elbow and forearm. If you were immobilized this pain is from not using the joints regularly. If you have had surgery, the pain is likely from the surgical process itself. Your pain may also be from concurrent soft tissue injury that occurred when you fractured your forearm. Your physical therapist will focus initially on relieving your pain. We may use modalities such as heat, ice, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the fracture site or anywhere along the arm or into the hand. In addition, we may massage the forearm, wrist, or elbow to improve circulation and assist with the pain.
The next part of your treatment will focus on regaining the range of motion, strength, and dexterity in your wrist, hand, elbow, and shoulder. If you have been immobilized, your arm will look and feel quite weak and atrophied after the period of immobilization. Your physical therapist will prescribe a series of stretching and strengthening exercises that you will practice in the clinic and also learn to do as part of your home exercise program. These exercises may include the use of rehabilitation equipment such as pliable balls or Theraband that provide added resistance for your hand and wrist. We may even give you exercises for your shoulder. The shoulder is the forearm’s link to the rest of the body so it needs to be strong and well controlled for the rest of the upper limb, including the hand, to work well. If necessary, your physical therapist will mobilize your joints. This hands-on technique encourages the stiff joints of your wrist and elbow to move gradually into their normal range of motion. Fortunately, gaining range of motion and strength after a forearm fracture occurs quickly. You will notice improvements in the functioning of your limb even after just a few treatments with your physical therapist. As your range of motion and strength improve, we will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows.
As a result of any injury, the receptors in your joints and ligaments that assist with proprioception (the ability to know where your body is without looking at it) decline in function. A period of immobility will add to this decline. Although your forearm and hand are not traditionally thought of as weight-bearing joints, even an activity such assisting yourself with your arms to get out of a chair or pulling a glass from a cupboard requires weight to be put through or lifted by your forearm and for your body to be proprioceptively aware of your limb. If you are an athlete, then proprioception of your upper extremity is paramount in returning you to sport after a forearm fracture. Your physical therapist will prescribe exercises for you to regain this proprioception. These might include exercises such rolling a ball on a surface with your hand, holding a weight up overhead while moving your shoulder, or pushups on an unstable surface. Advanced exercises will include exercises such ball throwing or catching. For athletes we will encourage exercises that mimic the quick motions of the sports or activities that you enjoy participating in.
Generally, the strength and stiffness one experiences after a forearm fracture responds very well to the physical therapy we provide at Combined Therapy Specialties. With our initial one-on-one physical therapy treatment along with the exercises of your home program, the strength, range of motion, and proprioception gradually improve towards near full recovery/function over a period of 3-6 months even though the actual final stages of bone healing won’t occur for another 6-12 months after that. If your pain continues longer than it should or therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon to confirm that the fracture site is tolerating the rehabilitation well and ensure that there are no hardware issues that may be impeding your recovery.
Combined Therapy Specialties provides services for physical therapy in Asheville.
Complications
What are the potential complications of this fracture?
Nonunion and malunion are common complications of this fracture but compartment syndrome does occur and has severe consequences.
Compartment Syndrome
The muscles of the forearm move the hand and fingers. When a fracture occurs the bone and muscle bleeds into the closed muscle compartments of the forearm. In some cases this is enough to raise the intra-compartment pressure high enough to stop blood flow to the muscle. As a result the muscle fibers may swell up and die (called necrosis). The swelling increases the pressure to cause a vicious cycle that may end in extensive damage to the muscles of the forearm. This condition is called a compartment syndrome. Untreated, this results in shortening and scarring of the muscles and loss of finger movement. The result is sometimes referred to as a claw hand, because the hand assumes the shape of a claw.
The cardinal sign of compartment syndrome is pain and tenderness of the forearm increased by pressure and by movement of the fingers. Since it is normal for the forearm to hurt after a fracture or after surgery it is often quite difficult to diagnose compartment syndrome.
Doctors and nurses pay a lot of attention to this problem and maintain a high index of suspicion. The treatment for compartment syndrome is immediate surgery to open up the muscle compartments and relieve the pressure. If this is done before any die off of the muscle fibers the outcome is satisfactory although the skin wound may be quite dramatic. Otherwise the outcome depends on the amount of muscle necrosis that has occurred.
Malunion
If the bones of the forearm heal with angulation, shortening, or rotation the fracture is said to be malunited. This is referred to as a malunion. The deformity may be significant enough to prevent full rotation of the forearm or it may be unsightly. Loss of rotation causes a problem with normal hand function so this problem usually requires treatment. The healed fracture is cut and the bone restored to normal length, rotation, and bowing.
Sometimes the extra bone laid down as part of the healing process causes a bony block which interferes with movement of the forearm and it has to be removed. In rare cases the radius actually heals to the ulna (this is called a cross union) and this completely prevents rotation of the forearm. Once the normal shape of the bone has been restored by surgery the fragments are fixed with internal fixation. Early movement to maintain the motion achieved by surgery is recommended.
Closed reduction may not result in anatomical alignment of the bones. Malunion is less common after operative treatment for two reasons. The first is that one aim of surgery is to restore normal alignment of the bones and this aim is usually achieved. The second is that the patient is encouraged to move the forearm once it has been fixed and this reduces the chances of cross-union or the development of a bony block.
Nonunion
A nonunion occurs when the healing process does not go on to completion. The first stage of healing results in scar tissue developing in the gap between the bone fragments and this normally turns to bone. If the gap is too big or there is significant movement at the site bone development may not occur and it stays as scar tissue (called soft callus). This failure of healing is also affected by the blood supply of the area and such general medical factors as smoking, diabetes, and alcoholism.
Diagnosis of nonunion is a judgment call by the orthopaedic surgeon. In his/her judgment the fracture will not heal without intervention. The treatment depends on the circumstances but the principle is to do surgery to freshen the bone ends, immobilize them and improve the biological environment by using bone graft to stimulate healing.
Nonunion is more common after nonoperative treatment. It is painful to put stress on an nonunited fracture so treatment is usually continued until healing has been accomplished. The long term consequence of multiple procedures to achieve healing may be scarring and loss of function of the forearm muscles with stiffness.
Painful Hardware
The plates and screws used to immobilize the fracture fragments may be tender. Sometimes they can be felt under the muscle layers and are sore when you rest your arm on a table. Very commonly there is a persistent ache that may be increased by weather changes. The reasons for this symptom are not known but removal of the hardware eliminates the problem.
Surgery to remove the plates and screws is often done once the bones have healed. However, there is a well recognized risk of refracture in the first few weeks after plate removal and patients are advised to be protective of their arm during this period.
Infection
After an open fracture or less commonly after surgery the wound may develop a bacterial infection. This results in increased pain, redness and swelling of the wound area with drainage of pus developing later. Early recognition and treatment of a wound infection may prevent it from becoming established and infecting the bone. Bone infection hinders healing and may be difficult to eliminate.
Treatment requires long-term use of antibiotics and surgery to remove all dead and contaminated tissue. The fixation is often left in so that the bone heals more quickly but hardware removal after healing is often required to finally eliminate the infection. With early aggressive treatment of infections the outcome is quite favorable.
Summary
A fracture of the forearm is a serious injury that results from moderate to severe accidents. The goal of treatment is to avoid the complications of malunion and nonunion and restore the best possible function of the limb. Surgery to straighten the bones and fix them in the correct position while they heal is a common way to treat this fracture and the eventual outcome from this treatment is good.
Portions of this document copyright MMG, LLC.